Uterine leiomyomas with bizarre nuclei: analysis of 37 cases after laparoscopic or open myomectomy
Deložní leiomyomy s bizarními jádry: analýza 37 prípadu po laparoskopické ci otevrené myomektomii
Cíl studie: Cílem studie byla analýza klinických výsledků pacientek, které podstoupily myomektomii jakožto fertilitu zachovávající operaci a byla u nich zjištěna diagnóza leiomyomu s bizarními jádry (LBJ).
Typ studie: Retrospektivní klinická studie.
Název a sídlo pracoviště: Gynekologicko-porodnická klinika VFN a 1. LF UK, Praha.
Metodika: V naší databázi byly vyhledány pacientky, u nichž byla v období od ledna 2002 do června 2017 provedena myomektomie s histologickým závěrem LBJ. Analyzovali jsme jejich klinická data získaná z lékařské dokumentace a korespondence s pacientkami.
Výsledky: Nalezeno bylo celkem 37 pacientek splňujících vstupní kritéria. Medián věku pacientek byl 34,0 let. Celkem 30 pacientek (81,1 %) podstoupilo operaci laparoskopickou, sedm (18,9 %) žen myomektomii laparotomickou. Peroperační vzhled myomu byl hodnocen jako typický ve 27 případech (73,0 %), v ostatních případech byl popsán jako abnormální či atypický. Klinická a reprodukční data z dalšího sledování byla získána od 35 žen, medián délky sledování byl 48 měsíců. U devíti pacientek (25,8 %) byla nutná další intervence pro myomy, přičemž ve dvou případech (22,2 %) byl nález histologicky hodnocen opět jako LBJ. Podíl žen, kterým se v celém souboru podařilo otěhotnět (pregnancy rate), byl 63,6 % a frekvence žen s živě narozeným dítětem (life birth rate) byl 33,3 %. Nezaznamenali jsme žádný případ vzdálené recidivy, maligní rekurence či úmrtí spojeného s diagnózou LBJ.
Závěr: Operace zachovávající dělohu u pacientek s LBJ se zdá jako bezpečná a racionální terapie u žen s přáním zachování fertility.
Klíčová slova:
atypický leiomyom – leiomyom s bizarními jádry – myomektomie – reprodukce
Authors:
B. Boudová 1; M. Mára 1; P. Dundr 2; M. Gregová 2; Z. Lisá 1; D. Kužel 1
Authors place of work:
Gynekologicko-porodnická klinika VFN a 1. LF UK, Praha, přednosta prof. MUDr. A. Martan, DrSc.
1; Ústav patologie VFN a 1. LF UK, Praha, přednosta prof. MUDr. P. Dundr, Ph. D.
2
Published in the journal:
Ceska Gynekol 2019; 84(5): 324-330
Category:
Retrospektivní studie
Summary
Objective: The aim of this study was to analyse the clinical outcome of patients with diagnosis of leiomyoma with bizarre nuclei (LBN) undergoing uterus saving surgery due to fertility preservation.
Design: Retrospective clinical study.
Setting: Department of Obstetrics and Gynaecology, First Faculty of Medicine, Charles University, General University Hospital, Prague.
Methods: This was a retrospective clinical study of patients with LBN diagnosis after myomectomy between January 2002 and June 2017 which were searched in our database. The data were obtained from medical documentation and from correspondence with patients.
Results: We identified 37 patients meeting the criteria in our database. The median age of the patients was 34.0 years. 30 patients (81.1%) underwent laparoscopic procedure, 7 (18.9.%) had open myomectomy. The perioperative appearance of fibroid was found normal in 27 cases (73.0%), in the rest the appearance was described somehow abnormal. The follow-up data were obtained from 35 women; the median follow-up time was 48 months. 9 patients (25.7%) needed re-intervention for fibroids with 2 specimens (22.2%) classified as LBN again. The overall pregnancy rate was 63.6% and life birth rate was 33.3%. We did not observe any distant recurrence of the disease or malignant recurrence or death related to the diagnosis.
Conclusion: Uterus sparing surgery for treatment of LBN seems to be safe and reasonable therapy for women wishing to preserve fertility.
Keywords:
reproduction – atypical leiomyoma – leiomyoma with bizarre nuclei – myomectomy
INTRODUCTION
Uterine leiomyomas are the most common benign pelvic tumors. They can be found in 40–60% of women in reproductive age and the presence of leiomyomas is increasing with age [14]. Since the reproductive behavior has changed and women have often not fulfilled their reproductive plans in their 30´s or even 40´s these days [4, 16], the need of uterine-preserving surgery will be raising. On the other hand, smooth muscle tumors of the uterus are not homogenous group and thus it is crucial to distinguish their histological pattern.
According to WHO histological classification of tumors 2014 beside leiomyosarcoma and smooth muscle tumor of uncertain malignant potential (STUMP) we can distinguish twelve different histological subtypes of benign leiomyomas (Table 1) [13]. Three of them (diffuse, intravenous, and metastasizing) are special for their unusual growing and that is why they were called growth pattern variants in 2003 classification [7]. The other nine histological subtypes are also interesting and different from standard leiomyomas because in some way they mimic malignancy. Leiomyoma with bizarre nuclei (LBN) is one of them and is characterized by significant (moderate to severe) cell atypias. In microscopic findings isolated or gathered bizarre cells with eosinophilic cytoplasm and nuclear changes like enlargement or hyperchromasia are usually found. Mitotic index is typically low and coagulative tumor cell necrosis has to be absent [13]. This histological variant used to be called atypical leiomyoma [7] but for the mostly observed benign behavior the term leiomyoma with bizarre nuclei or symplastic leiomyoma is now preferred. There is couple of studies looking at the behavior of the LBN but data on fertility saving management (myomectomy) of these tumors are lacking. In our paper, we have focused on clinical outcomes of these patients like: rates of recurrences, re-interventions and pregnancies.
![WHO classification of tumours of the uterine corpus –
smooth muscle tumors 2014 [13]](https://www.cs-gynekologie.cz/media/cache/resolve/media_object_image_small/media/image_pdf/04cfbb2a76a35e3d509f5951f0766fe1.png)
MATERIALS AND METHODS
We conducted a retrospective clinical study. Patients with laparoscopic or open myomectomy performed between January 2002 and June 2017 and pathological findings containing the signs of LBN were searched in our database. All histology sections underwent expert second reading for confirmation of the diagnosis according to WHO classification 2014.
In our department, the special team of reproductive surgery has been established focusing on surgical treatment of fibroids, which makes the evaluation of subjective parameters (such as appearance of tumor) during surgery less heterogeneous. For extraction of fibroids during the laparoscopic surgery we commonly use laparoscopic power morcellation and only when the tumor has suspicious appearance (necrotic, disintegrating tissue), then the endoscopic retrieval bag is used to avoid potential dissemination of tumor cells.
After identifying the patients with LBN diagnosis we reviewed accessible medical documentation about the surgery, postoperative clinical course, and possible further data on re-admissions or re-interventions in our department. For information about actual health and follow-up we contacted all patients by email or phone. After all we documented and analyzed the following data: age at the time of surgery, preoperative symptoms, history of previous surgery of the uterus, number, size and the perioperative appearance of the fibroids, use of laparoscopic power morcellation, need of re-interventions due to recurrence of leiomyoma and their pathological results, actual clinical symptoms, length of follow-up and eventual post-myomectomy reproductive outcomes. We excluded women with follow-up shorter than six months for calculation of pregnancy and life birth rate. The study protocol was approved by the Ethics Committee of the General University Hospital in Prague.
RESULTS
After searching in our database, out of 1680 patients with myomectomy performed in our department 37 patients (2.2%) met the criteria of LBN. The age of the women at time of the surgery ranged from 23 to 45 years (median 34.0 years, average 34.4 years). Out of 37 patients, 25 (67.6%) had fibroid-related symptoms before surgery: hypermenorrhea in 11 women (29.7%), dysmenorrhea in eight (21.6%), combination of hypermenorrhea and dysmenorrhea in four patients (10.8%), hypermenorrhea and lower abdominal pressure in one (2.7%) and only pressure in one woman (2.7%). Twelve patients were asymptomatic and the surgery was indicated for diameter of the dominant fibroid 5cm or larger on the ultrasound in 11 cases and for secondary infertility in one case. Three patients with diagnosis of LBN underwent previous myomectomy with histological findings of typical leiomyoma in one and cellular leiomyoma in two cases.
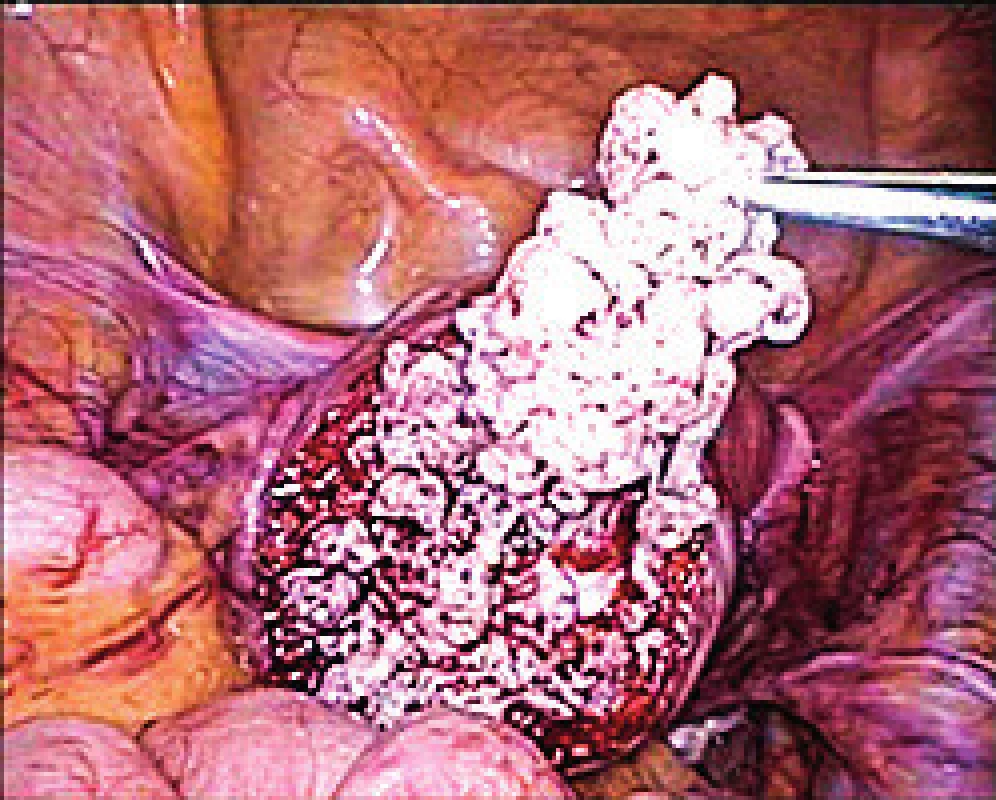
Out of 37 patients 30 (81.1%) had laparoscopic procedure (without any conversion to laparotomy) and seven women (18.9%) underwent elective open myomectomy due to the size and/or number of fibroids. Average diameter of the largest leiomyoma was 5.7 cm (from 4 up to 10 cm) and we enucleated 2.5 leiomyomas per surgery in average ranging from 1 to 10 leiomyomas. There was logically no problem with tumor extractions in open procedures. From 30 laparoscopic myomectomies, we used the retrieval bag only twice (6.6%) in tumors with suspicious necrotic appearance (Fig. 1). In all other cases we used laparoscopic power morcellation. Completely normal perioperative appearance of leiomyomas was described in 27 cases (73.0%), in the rest of them we found the appearance somehow abnormal, which meant that the fibroid had at least one of the following signs: soft, disintegrating, hard to separate from the health tissue, containing necrosis or other type of tissue regression.
During the follow-up we gathered reliable information about 35 patients which means that two patients were lost during the follow-up. The median follow-up period was 48 months (1–130 months) with 68,6% women with follow-up three years and longer.
Nine patients (25.7%) needed re-intervention, while seven of them had some fibroid-related symptoms, one patient had growing fibroid 5cm in diameter and one patient decided for radical treatment. Two women underwent open myomectomy, three laparoscopic myomectomy and four had hysterectomy. Two specimens (22.2%) were classified again as leiomyoma with bizarre nuclei, and one (11.1%) as mitotically active. The other six histological findings (66.7%) were evaluated as regular leiomyomas.
Out of 35 women with actual follow-up, 17 patients (48.6%) are without clinical symptoms and without ultrasound finding of recurrent leiomyoma. 15 women (42.8%) have fibroid on the ultrasound (with typical echo-structure for leiomyomas) but no symptoms and three patients (8.6%) have minor symptoms along the ultrasound finding of fibroids, but no re-intervention until now.
In terms of reproductive outcomes of women with LBN-myomectomy we have observed eight cases of miscarriage, four cases of termination of pregnancies on patient´s request, one case of ectopic pregnancy, eight cases of cesarean section with only one of them preterm at week 36, one woman with two cesarean sections, two cases of spontaneous term delivery, one woman with two spontaneous term deliveries and one patient got pregnant recently. The overall pregnancy rate was 63.6% and life birth rate was 33.3%.
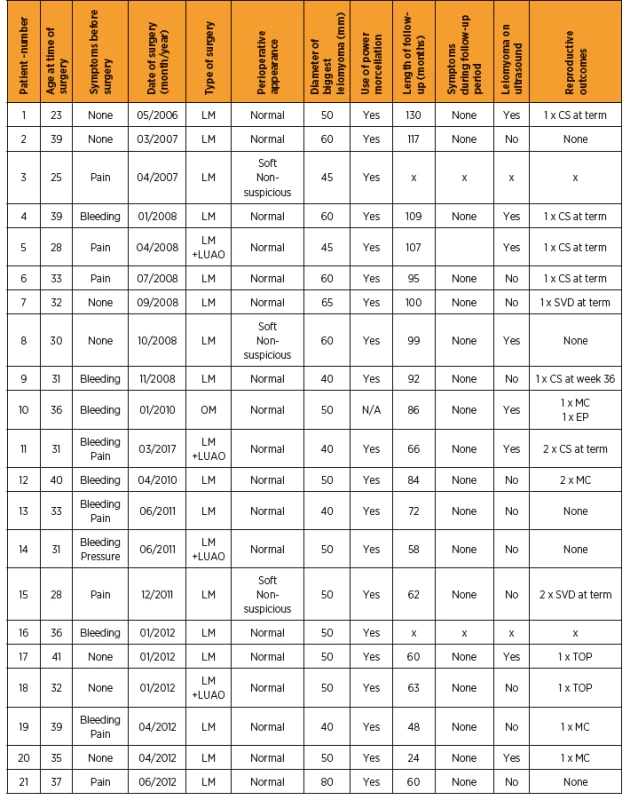
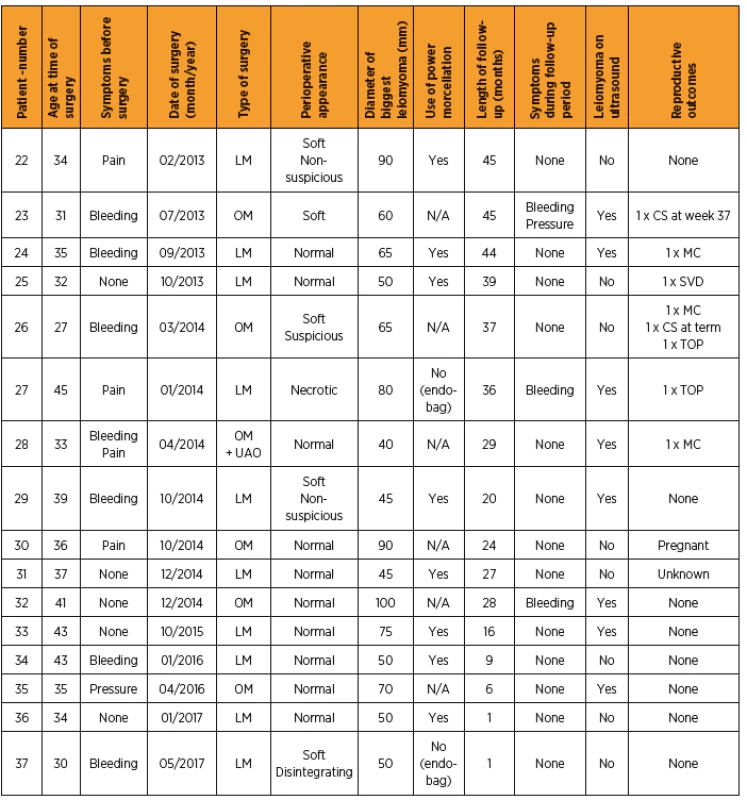
All relevant data are available in chronological flowchart of the patients (Table 2).
DISCUSSION
Uterine masses are not homogenous group of tumors. If we take just the tumors from smooth muscle cells we can distinguish three subgroups according to the biological behavior.
The malignant variant of the smooth muscle tumors are leiomyosarcomas. Their diagnosis is based on the evaluation of three basic histological features: nuclear atypias, the number of mitoses, and the presence of coagulative type of necrosis, respectively. These criteria are somewhat different for the most common spindle cell type of leiomyosarcoma and for the epithelioid or myxoid type [7, 10]. Uterine leiomyosarcoma is aggressive type of tumor, but fortunately it is rare, it comprises about 1 - 2% of all uterine malignancies [3, 11, 13]. The recurrence rate ranges in the literature from 53% to 71% [3] and 5-year survival rate is 15 - 70% [8, 11, 13] depending on the stage of disease.
Somewhere between the malignant and benign variant of the smooth muscle tumors is a heterogeneous group called STUMP which can be also called atypical smooth muscle neoplasm according to WHO classification 2014 [13]. STUMP is characterized as a tumor from smooth muscle cells which is fulfilling criteria of neither leiomyosarcoma nor benign leiomyoma or its variants. The recurrence rate varies in literature from 7% to 27% [5, 15] and overall 5-year survival is 92–100% [15].
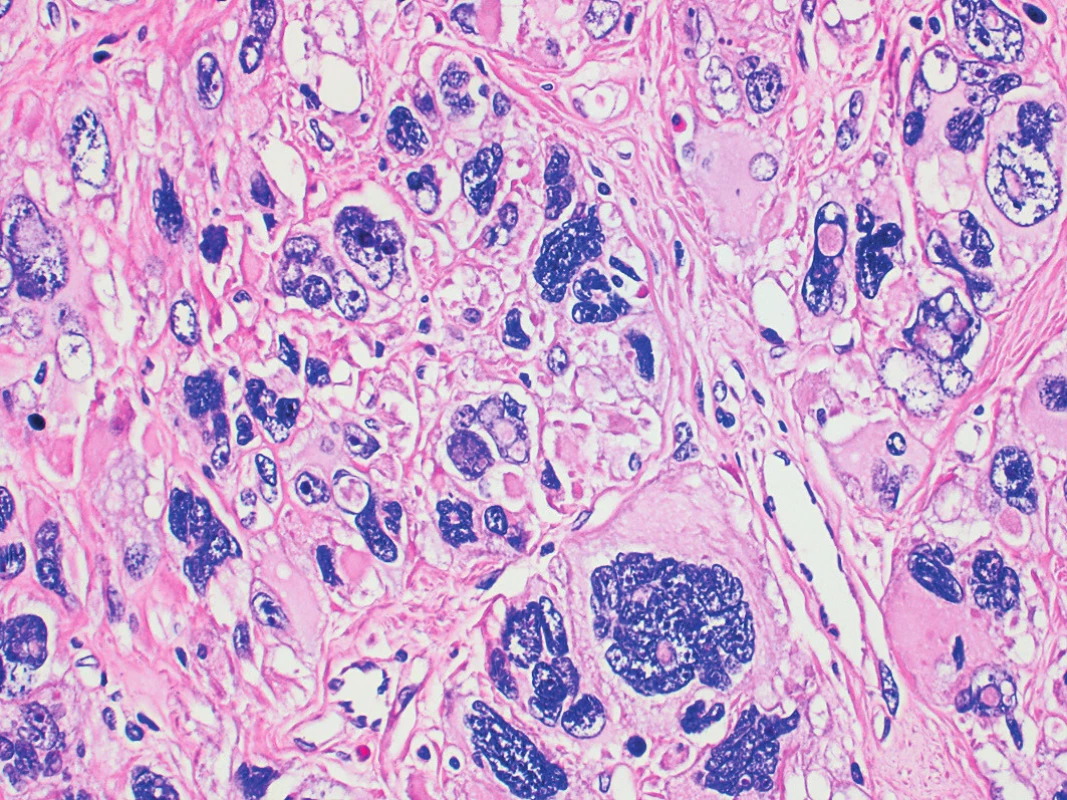
After all we have benign leiomyomas and their histological variants. LBN is one of the most studied subgroup because of its ominous microscopic appearance with presence of nuclear atypias, which are commonly high grade (Fig. 2). Most recent studies are confirming its benign potential with no recurrence after hysterectomy or myomectomy (n = 59) in Croce´s study from 2014 [2], with 1 recurrence after hysterectomy (n = 34) reported by Ly et al. in 2013 [12] and 18% of recurrences after myomectomy from the same study (n = 17), and 1 recurrence of leiomyoma but not the LBN after hysterectomy (n = 22) and no recurrence after myomectomy (n = 8) in Kefeli´s study from 2017 [9]. On the other hand, all those studies have analyzed patients mostly after hysterectomy and only few patients after uterus preserving procedure.
Since the ultrasound imaging has weak specificity for differentiating of atypical findings in uterus fibroids [1] it is hard or impossible to say the real recurrence rate for LBN in woman with fibroids not undergoing re-intervention. Presence of fibroid-like uterine mass on the ultrasound does not necessarily mean the recurrence of LBN. This can be demonstrated by pathological findings of women who underwent re-intervention in our study rating 66.7% of cases as standard leiomyoma. It looks that the recurrence of fibroids (on the ultrasound imaging with or without fibroid related symptoms) in our study (51.4%) with median follow-up 4 years does not significantly differ from the recurrence of common leiomyoma from other studies [6, 18]. On the other hand we didn´t register any malignant pelvic or distant recurrence or metastasis or even death related to the disease which was one of the main purposes of this study. In the light of these facts uterus saving management of patients with LBN seems to be feasible and safe.
The uterus preserving procedures are done mainly for remaining of reproductive functions, therefore our interest has also been focused on reproductive outcomes of this specific subgroup of patients with LBN. Even though we don´t know the actual effort of all our patients, neither we know the whole reproductive status of the couple, we still got some relevant data for comparison. According to our results the reproductive outcome is not affected by histology pattern of LBN since the pregnancy rate and life birth rate was in range of the literature [17].
CONCLUSION
Our study with 37 women with myomectomy and histological result of LBN is showing that uterus saving surgery can be safe alternative for young women wishing to preserve fertility. It is in consensus with literature that LBN is benign variant of leiomyomas and malignant recurrences are very rare. We suppose that for woman with diagnosis of LBN no special management or follow-up is necessary.
The work was supported by Charles University in Prague (UNCE 204065 and PROGRES Q28/LF1).
MUDr. Barbora Boudová
Gynekologicko-porodnická klinika
VFN a 1. LF UK
Apolinářská 18
128 00 Praha 2
e-mail: Barbora.Boudova@vfn.cz
Zdroje
1. Benson, C., Miah, AB. Uterine sarcoma – current perspectives. Int J Womens Health, 2017, 9, p. 597–606.
2. Croce, S., Young, RH., Oliva, E. Uterine leiomyomas with bizarre nuclei: a clinicopathologic study of 59 cases. Am J Surg Pathol, 2014, 38(10), p. 1330–1339.
3. D‘Angelo, E., Prat, J. Uterine sarcomas: a review. Gynecol Oncol, 2010, 116(1), p. 131–139.
4. Eurostat. Fertility statistics. 2017. Available at http://ec.europa.eu/eurostat/statistics-explained/index.php/Fertility_statistics#Further_Eurostat_information. Accessed January 12, 2018.
5. Guntupalli, SR., Ramirez, PT., Anderson, ML., et al. Uterine smooth muscle tumor of uncertain malignant potential: a retrospective analysis. Gynecol Oncol, 2009, 113(3), p. 324–326.
6. Hanafi, M. Predictors of leiomyoma recurrence after myom-ectomy. Obstet Gynecol, 2005, 105(4), p. 877–881.
7. Hebrickson, MR., Tavassoli, FA., Kempson, RL., et al. Mesenchymal tumours and related lesions. In: Tavassoli, FA., Devilee, P. (eds). Pathology and genetics of tumours of the breast and female genital organs. 3th ed. Lyon, IARC Press, WHO, 2003, p. 233–241.
8. Kapp, DS., Shin, JY., Chan, JK. Prognostic factors and survival in 1396 patients with uterine leiomyosarcomas: emphasis on impact of lymphadenectomy and oophorectomy. Cancer, 2008, 112(4), p. 820–830.
9. Kefeli, M., Caliskan, S., Kurtoglu, E., et al. leiomyoma with bizarre nuclei: clinical and pathologic features of 30 patients. Int J Gynecol Pathol, 2018, 37(4), p. 379–387.
10. Kempson, RL., Hendricson, MR. Smooth muscle, endometrial stromal, and mixed Müllerian tumours of the uterus. Mod Pathol, 2000, 13(3), p. 328–342.
11. Kim, WY., Chang, SJ., Chang, KH., et al. Uterine leiomyosarcoma?: 14-year two-center experience of 31 cases. Cancer Res Treat, 2009, 41(1), p. 24–28.
12. Ly, A., Mills, AM., McKenney, JK., et al. Atypical leiomyomas of the uterus: a clinicopathologic study of 51 cases. Am J Surg Pathol, 2013, 37(5), p. 643–649.
13. Oliva, E., Carcangiu, ML., Carinelli, SG., et al. Tumours of the uterine corpus: mesenchymal tumours. In: Kurman, RJ., Carcangiu, ML., Herrington, CS. (eds). World Health Organisation Classification of Tumours of the Female Reproductive Organs. 4th ed. Lyon: International Agency for Research on Cancer, WHO, 2014, p. 135–147.
14. Parker, WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril, 2007, 87(4), p. 725–736.
15. Peters, WA. 3rd, Howard, DR., Andersen, WA., Figge, DC. Uterine smooth-muscle tumors of uncertain malignant potential. Obstet Gynecol, 1994, 83(6), p. 1015–1020.
16. Rodička a novorozenec 2014–2015. Praha: Ústav zdravotnických informací a statistiky ČR, 2017.
17. Shin, DG., Yoo, HJ., Lee, YA., et al. Recurrence factors and reproductive outcomes of laparoscopic myomectomy and minilaparotomic myomectomy for uterine leiomyomas. Obstet Gynecol Sci, 2017, 60(2), p. 193–199.
18. Yoo, EH., Lee, PI., Huh, CY., et al. Predictors of leiomyoma recurrence after laparoscopic myomectomy. J Minim Invasive Gynecol, 2007, 14(6), p. 690–697.
Štítky
Dětská gynekologie Gynekologie a porodnictví Reprodukční medicínaČlánek vyšel v časopise
Česká gynekologie

2019 Číslo 5
Nejčtenější v tomto čísle
- Syndrome Mayer-Rokitansky-Küster-Hauser – uterine and vaginal agenesis: current knowledge and therapeutic options
- ERAS protocol in gynecologic oncology
- First-trimester screening for preeclampsia
- Uterine rupture during pregnancy
