Laparoscopic sacrocolpopexy using Seratex Slimsling: pilot study
Laparoskopická sakrokolpopexe pomocí materiálu Seratex Slimsling: pilotní studie
Cíl práce: Popsat novou techniku laparoskopické sakrokolpopexe pomocí materiálu Seratex Slimsling.
Typ práce: Pilotní studie.
Název a sídlo pracoviště: Gynekologicko-porodnické oddělení, Nemocnice Vyškov p.o.; Porodnicko-gynekologická klinika, Lékařská fakluta UP a Fakultní nemocnice Olomouc.
Metodika: Pomocí laparoskopicky inzerovaného materiálu Seratex Slimsling jsme v období od listopadu 2018 do června 2019 v rámci pilotní studie provedli sakrokolpopexi u 12 pacientek s pánevním prolapsem. Všechny pacientky byly operovány na jednom pracovišti stejným operatérem se zkušeností s pokročilou laparoskopickou operační technikou. V pilotním souboru pacientek jsme sledovali věk, paritu, BMI, provedení předchozí hysterektomie, operační čas, krevní ztráty, typ konkomitantní operace, délku hospitalizace, výskyt peroperačních a pooperačních komplikací.
Výsledky: Pacientky zařazené do pilotní studie měly věk 53,2 ± 10,0 (34–74) let, BMI 24,7 ± 4,2, paritu 1,92 (z toho v 95,7 % se jednalo o vaginální porod) a v pěti případech (41,7 %) byla provedena přechozí hysterektomie. Průměrná délka operace byla 58,4 ± 6,6 min u případů bez hysterektomie a 102 ± 4,9 u pacientek s konkomitantní hysterektomií. Průměrná krevní ztráta byla 93 ± 78,8 ml a délka hospitalizace 5,25 ± 0,72 dní. Během žádné operace nedošlo k poranění velkých cév nebo ureterů a žádná z operací nebyla konvertována na laparotomii. U jedné z pacientek došlo ke sklouznutí implantátu z oblasti sakrouterinních vazů a následné recidivě prolapsu poševního pahýlu tři měsíce po primární operaci. Pacientka byla následně reoperována půl roku po primární operaci stejnou technikou a dosud je již bez obtíží. Ve sledovaném pooperačním období nedošlo u žádné z pacientek k protruzi implantátu ani k výrazným dyspareuniím či dyskomfortu a kromě výše zmíněné pacientky ani k selhání metody.
Závěr: Laparoskopie má v gynekologické operační technice pro pánevní prolaps od roku 1993 své nezastupitelné místo. Pomocí materiálu Seratex Slimsling je možné provést laparoskopickou sakrokolpopexi s vysokou úspěšností a minimálním výskytem komplikací.
Klíčová slova:
prolaps – laparoskopická sakrokolpopexe – Seratex Slimsling
Authors:
M. Vašíček 1; R. Pilka 2; J. B. Eim 1
Authors place of work:
Department of Obstetrics and Gynecology, Vyškov Hospital, head J. B. Eim
1; Department of Obstetrics and Gynecology, Faculty of Medicine and Dentistry, Palacky University, University Hospital, Olomouc, head Prof. R. Pilka, M. D., Ph. D.
2
Published in the journal:
Ceska Gynekol 2019; 84(6): 412-417
Category:
Pilotní studie
Summary
Objective: To describe a new technique of laparoscopic sacrocolpopexy using material Seratex Slimsling.
Design: Pilot study.
Setting: Department of Obstetrics and Gynecology, Vyškov Hospital; Department of Obstetrics and Gynecology, Faculty of Medicine and Dentistry, Palacky University, University Hospital Olomouc.
Methods: Using a laparoscopically inserted Seratex Slimsling material, we performed a sacrocolpopexy in 12 patients with pelvic prolapse between November 2018 and June 2019. All patients were operated at the same workplace by the same surgeon with experience in advanced laparoscopic surgery. We monitored age, parity, BMI, previous hysterectomy, surgical time, blood loss, type of concomitant surgery, length of hospitalization and incidence of peroperative and postoperative complications in the pilot group of patients
Results: Patients included in the pilot study were 53.2 ± 10.0 (34–74) years old, BMI 24.7 ± 4.2, parity 1.92 (95.7% of whom were vaginal births) and in 5 cases (41.7%) previous hysterectomy was performed. The mean duration of surgery was 58.4 ± 6.6 min in cases without hysterectomy and 102 ± 4.9 in patients with concomitant hysterectomy. The mean blood loss was 93 ± 78.8 ml and the length of hospitalization was 5.25 ± 0.72 days. There was no injury to large vessels or ureters during any operation and none of the operations was converted to laparotomy. In one case, the implant slipped from the sacrouterine ligaments area and subsequently the vaginal stump prolapse recurred three months after the primary operation. The patient was re-operated six months after the primary operation using the same technique and has been without any problems until now. In the monitored postoperative period, we did not notice any protrusion of the implant or significant dyspareunias or discomfort in any of the patients. Apart from one patient mentioned above, the method did not fail.
Conclusion: Laparoscopy has had an irreplaceable role in gynecological surgery for pelvic prolapse since 1993. It is possible to perform laparoscopic sacrocolpopexy with high success rate nad minimal incidence of complications with the use of Seratex Slimsling.
Keywords:
prolapse – laparoscopic sacrocolpopexy – Seratex Slimsling
INTRODUCTION
Pelvic organ prolapse is a common problem in women. It is associated with an increase in morbidity and a significant decrease in the quality of life [5]. It is a specific vaginal segment defect associated with the descent of the vagina and affiliated pelvic organs. The pelvic structures that may be affected by the prolapse include the uterus, vaginal apex, anterior or posterior vaginal wall [13]. The treatment of pelvic organ prolapse is performed in particular by the surgical approach [9]. Sacrocolpopexy is a method of prolapse correction that restores the pelvic anatomy by attaching supporting fibrous structures to the sacrum [3]. There are three basic surgical approaches for sacrocolpopexy: transabdominal, laparoscopic and robotic. In 1957, Arthure and Savage from London and Ameline and Huguier from Paris published the first literature on abdominal sacropexy methods. The following year, Huguier and Scali published a series of results for this surgical technique [7]. A systematic review of Cochrane database concluded that abdominal sacropexy is associated with less recurrence and risk of material protrusion in the vaginal space and less dyspareunia than vaginal sacrospinous fixation [9]. In contrast, open abdominal sacrocolpopexy was associated with longer operating time, longer hospital stays, and higher costs than vaginal sacrospinous fixation. Laparoscopic sacrocolpopexy was shown to be able to reduce some disadvantages of open approach [10].
The first laparoscopic sacrocolpopexy dates back to 1993 and has been reported by a number of authors. It has shown comparable medium-term efficacy to traditional open-ended approaches with reduced pain, reduced intraoperative blood loss and hospital stay, and shorter recovery times [5]. The da Vinci surgical robotic system (Intuitive Surgical Inc., Sunnyvale, CA) offers advantages over conventional laparoscopy, with three-dimensional imaging, instruments with seven degrees of freedom to emulate human wrist movement, and tremor filtration. These benefits have made complex laparoscopic interventions more accessible to surgeons with limited laparoscopic experience. Initial reports with a short term (up to one year) follow-up for robotic sacrocolpopexy demonstrated results comparable to those seen with abdominal approach [1]. Important disadvantages orcomplications to consider for sacrocolpopexy with either an open or a minimally invasive approach include operation time and mesh erosion, often depending on the type of material used for the treatment.
The aim of the current retrospective pilot study is to evaluate the safety and short term outcomes mesh-less and dissection-less anchoring system Seratex Slim sling for pelvic floor apical repair as done by laparoscopy. To our knowledge this is the first report on a clinical use of this material.
MATERIAL AND METHOD
This is a retrospective pilot study of a group of 12 patients operated in the Vyškov hospital between November 2018 and June 2019. The operation has always been performed using material from Serag company – Seratex Slimsling. Only patients with symptomatic stage prolapse II and more were operated on (POP-Q; Bump 1996). Three patients from the total group underwent concurrent laparoscopic assisted vaginal hysterectomy, four patients had a uterine suspension and five patients had previously undergone hysterectomy.
Preparation before surgery
All patients underwent vaginal and abdominal ultrasound examination before surgery to exclude serious gynecological pathology. No preoperative intestinal preparation or laxative was administered. After introduction to general anesthesia, a catheter was always inserted into the bladder. After vaginal disinfection, the uterine manipulator was inserted, and a blunt vaginal probe was inserted in the case of patients with previes hysterectomy. All patients received 1.5 g of ampicillin/sulbactam i.v. perioperatively and in the early postoperative period.
Surgical technique
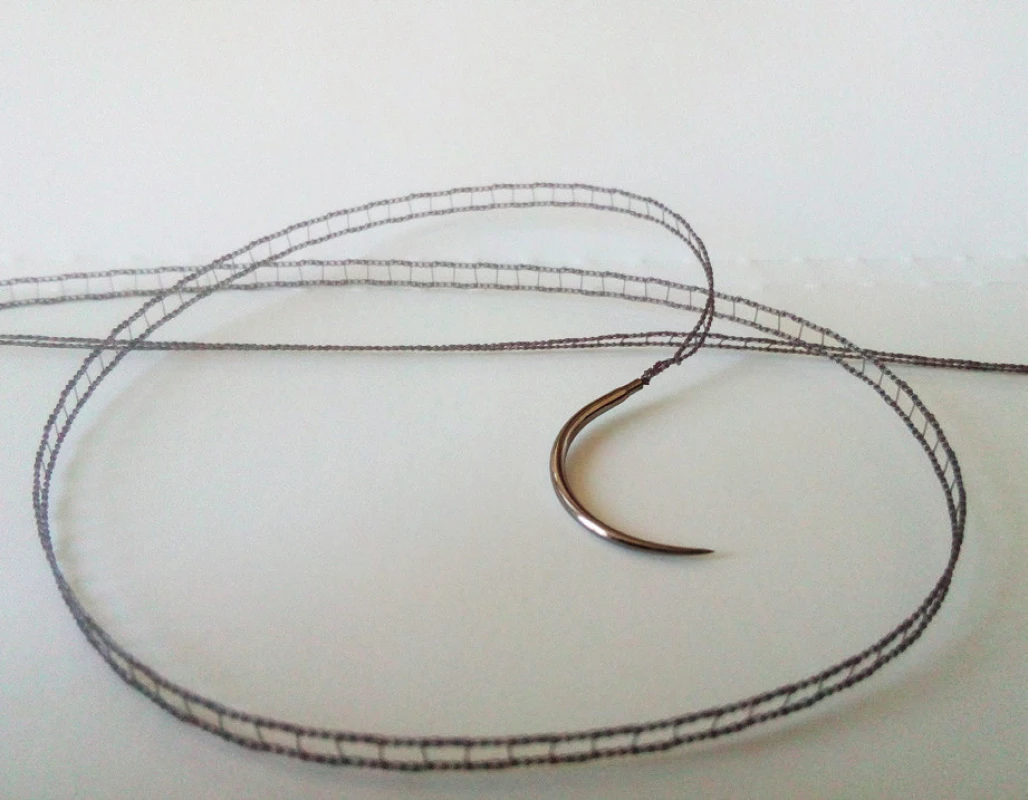
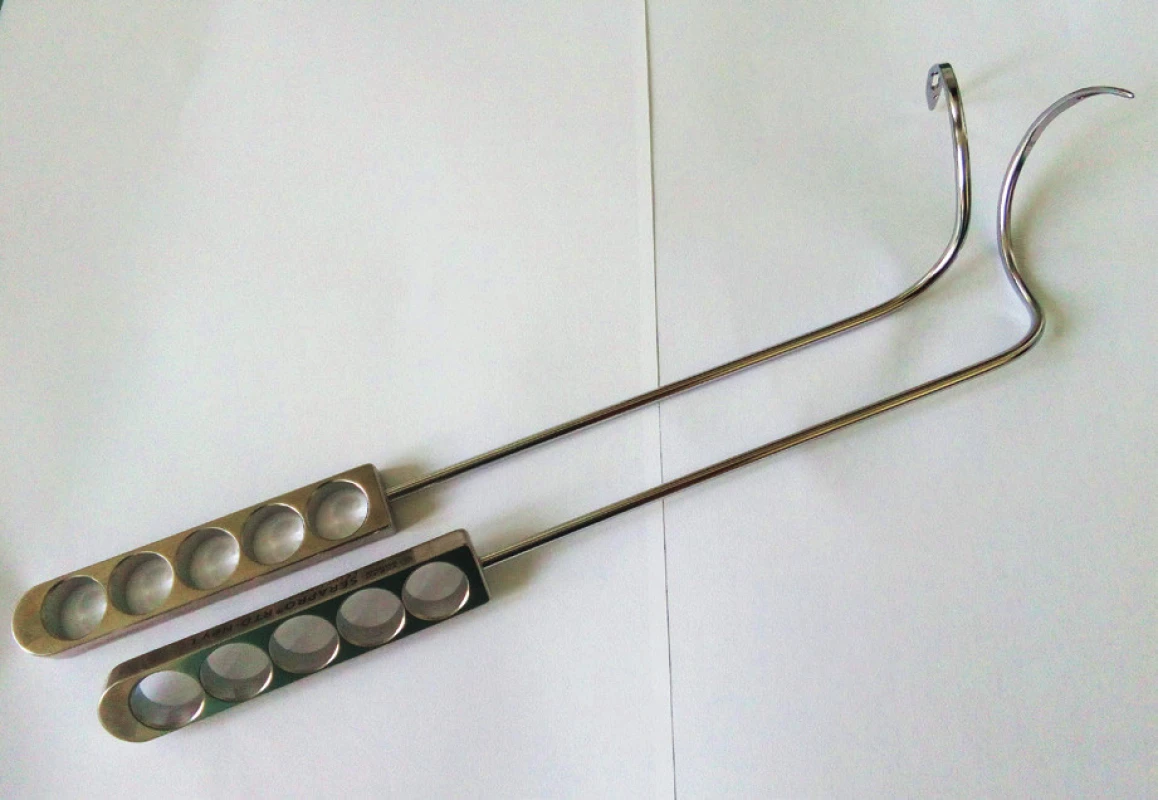
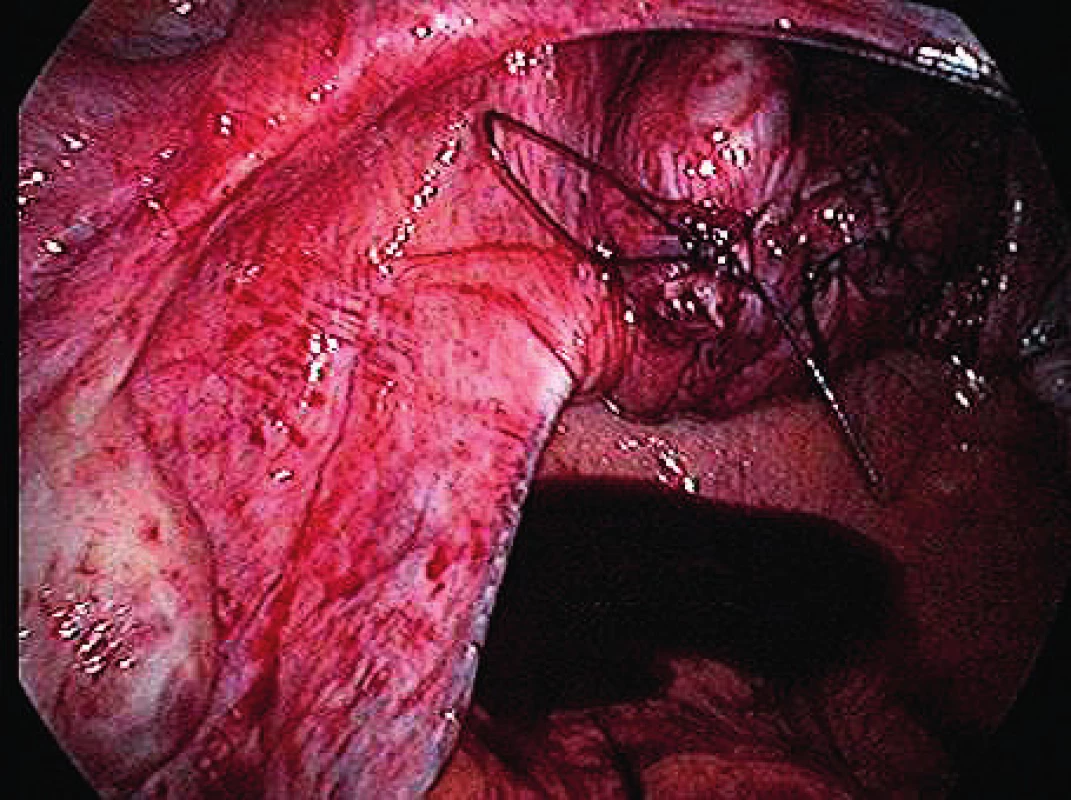
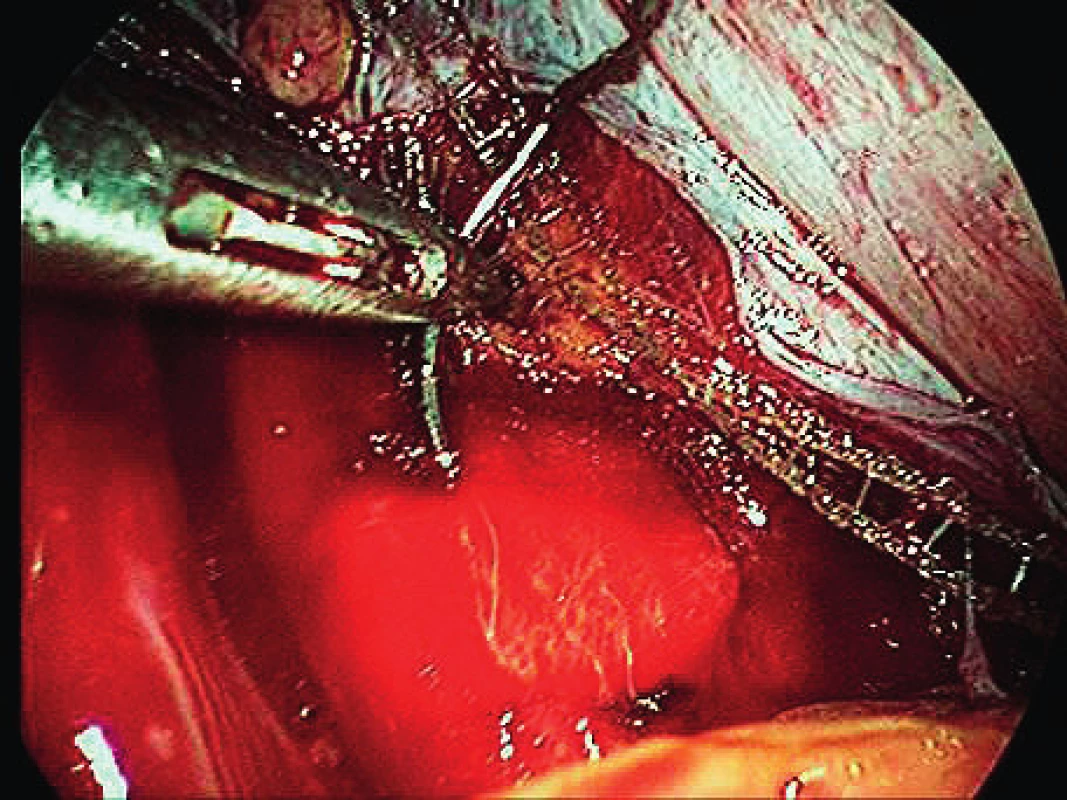
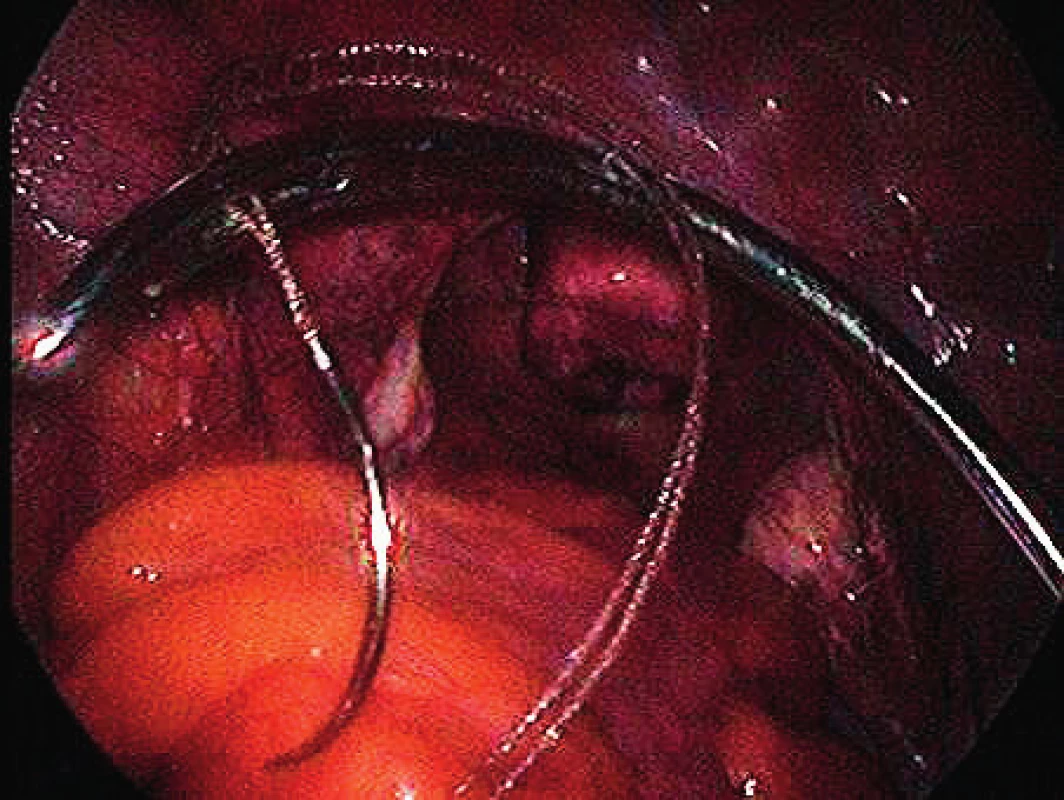
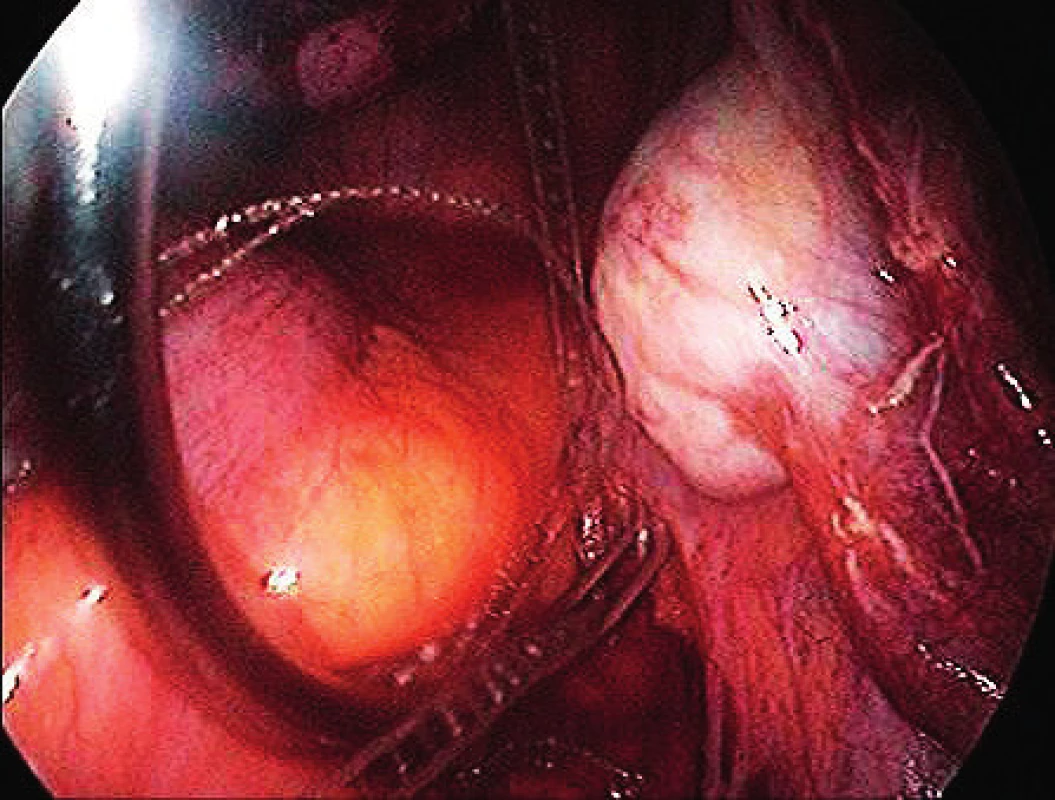
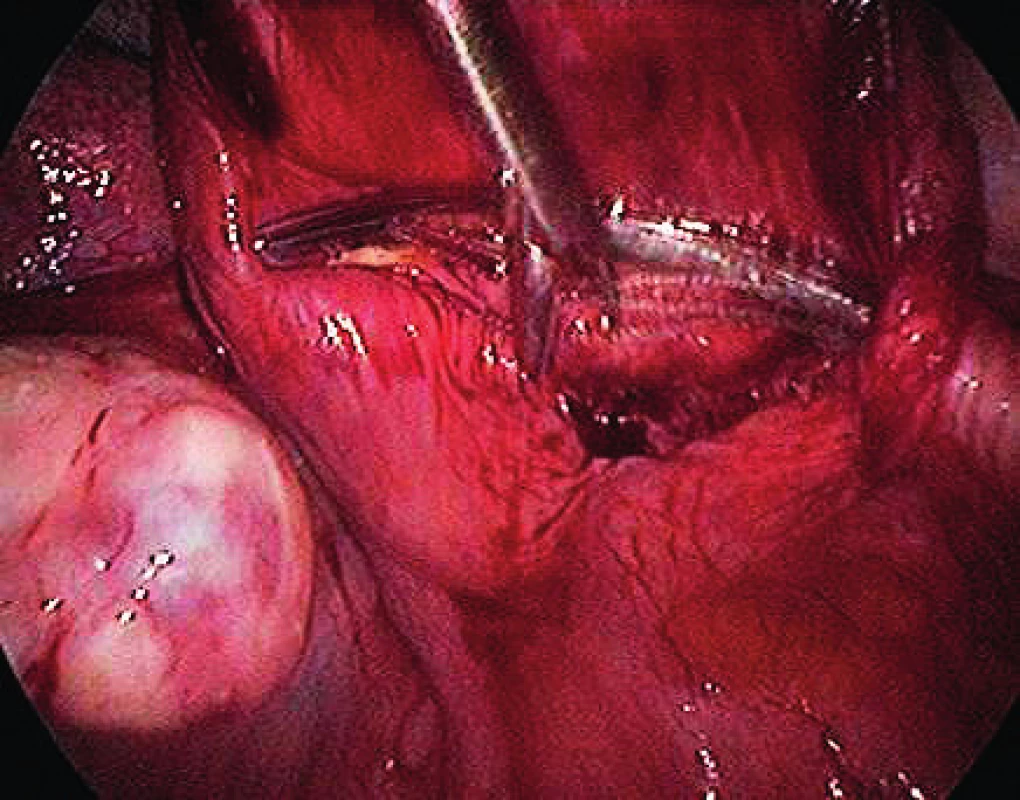
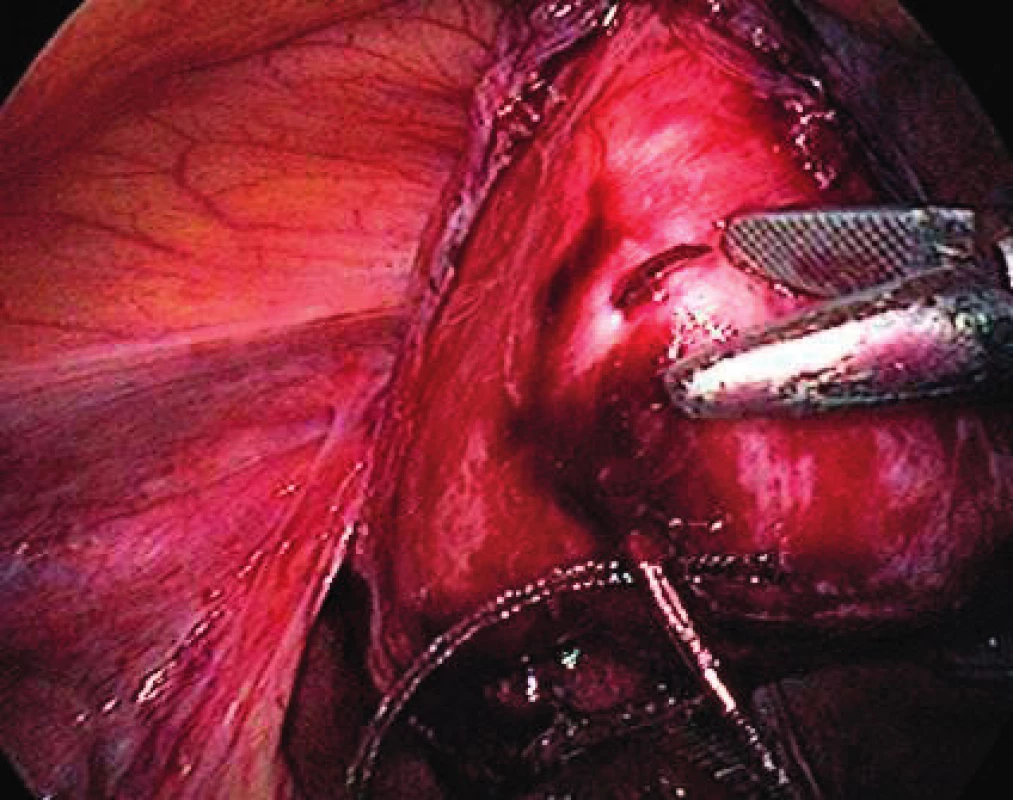
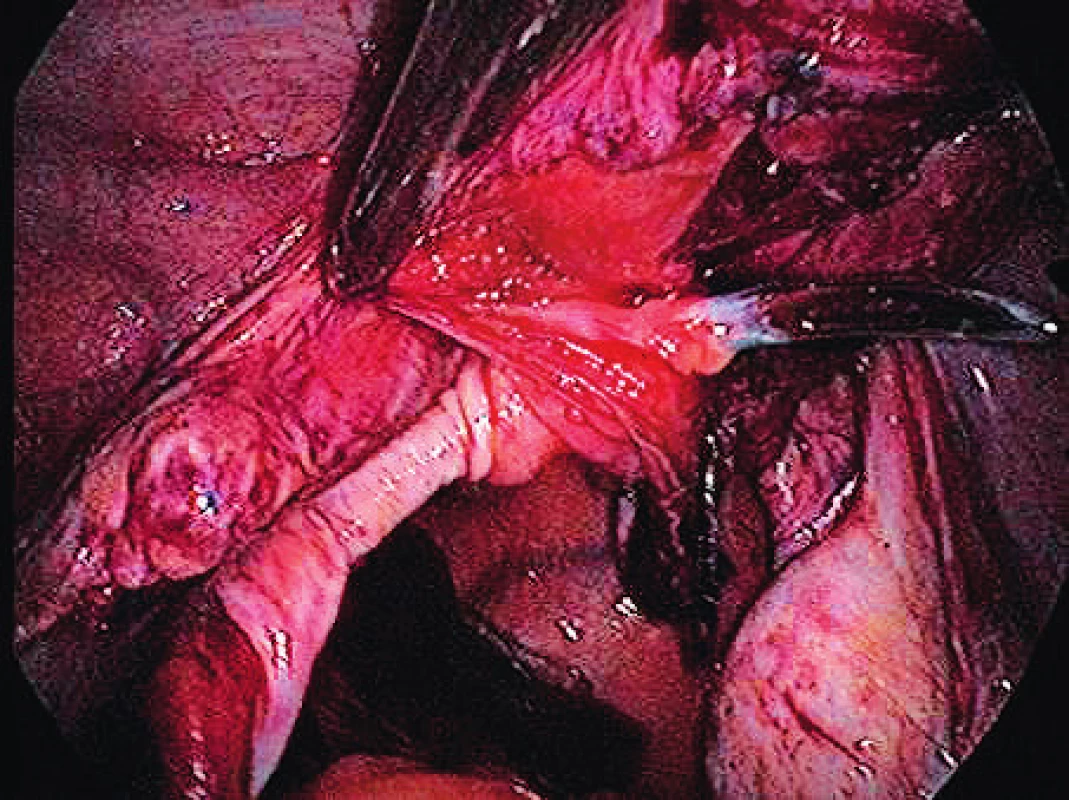
The surgical technique, the implant used, the instruments and the pilot study were based on the work of MUDr. Jörg Neymeyer, Chief Medical Officer of Charité – Universitätsmedizin Berlin. After the pneumoperitoneum formation, we use a 5 mm / 30° laparoscop inserted transumbilically. We introduce only two additional 5 mm trocars laterally in the hypogastrium. To prevent injury, we visualize iliac vessels and ureters on both sides as well as the pelvic cavity to exclude macroscopic pathology in this area. We start with peritoneum dissection and exposition of praesacral connective tissue on the lateral sides of the promotorium. We only dissect peritoneum in the area required for preparation and do not continue distally. We carry out the preparation gently to expose the ligamentum longitudinale anterius. Afterwards we dissect peritoneum to expose the vaginal stump. In case of patients with uterus, we insert the implant to the attachement of sacroucterine ligaments to the cervix. The Seratex Slimsling implant consisting of a combination of sewing material and textile implant is then inserted into the abdominal cavity (Fig. 1). We use a needle to fix the cranial part of the implant to the presacral ligament (Fig. 3). Afterwards, we insert the Serapro RTD abdominal instrument into the abdominal cavity through the right port (Fig. 2), with the needle and implant (Fig. 4). Subsequently, with the Serapro RTD instrument, we penetrate laterally through the dissection opening at the promontory and (Fig. 5) continue subperitoneally to the second dissection opening on the cervix or vaginal stump laterally (Fig. 6). Then we release the implant with the needle from the end of the instrument and remove the instrument. Using a needle, we fix the ladder net to the vaginal stump or cervix, to avoid penetration of the vaginal mucosa (Fig. 7). Using the Serapro RTD tool on the left, we work similarly as on the right (Fig. 8) and fix the implant laterally into the praesacral connective tissue. Finally, we peritonealize the implant with absorbable suture on the vaginal stump or cervix (Fig. 9). With respect to small surgical field anterior to sacral bone we do not close peritoneum of this area routinelly. The procedure can be finished with concomitant anterior or posterior vaginal repair when needed. In three patients, we combined the procedure with laparoscopically assisted vaginal hysterectomy. First the hysterectomy was done in usual way followed by implant insertion strictly avoiding the suture of vaginal stump after hysterectomy.
RESULTS
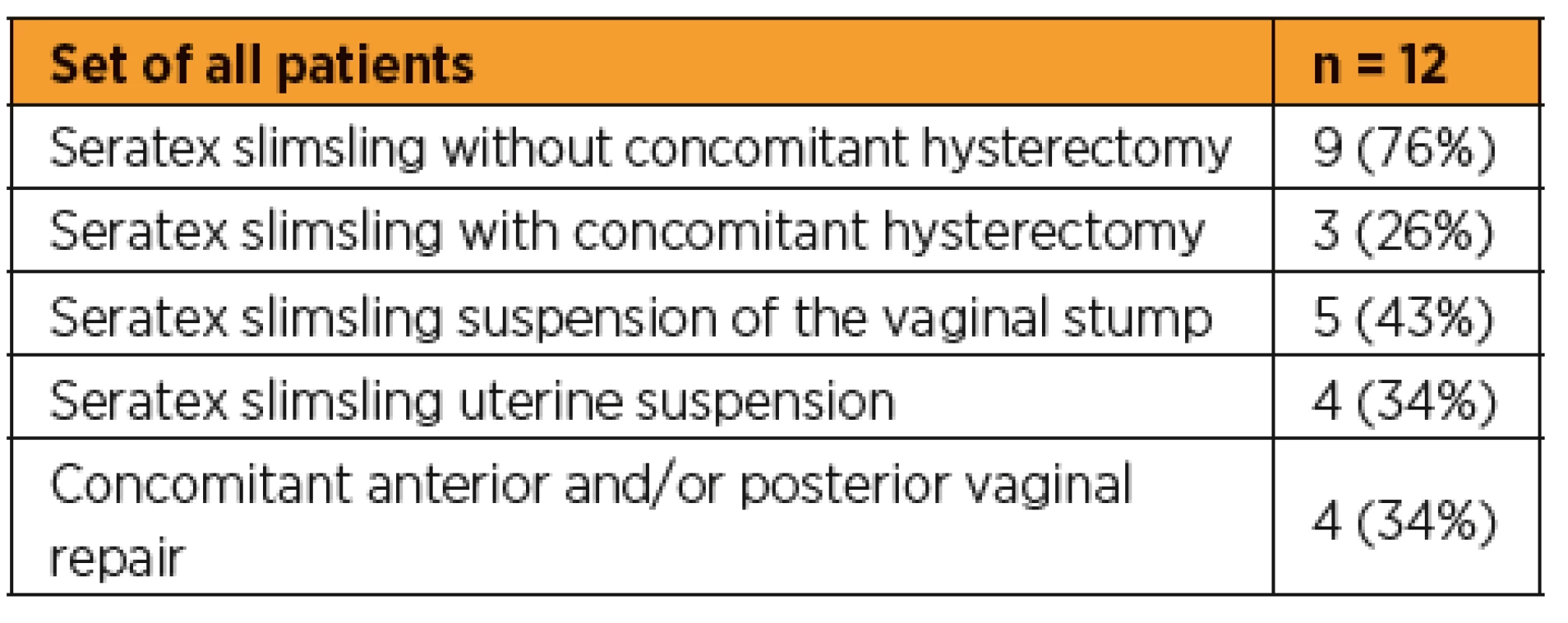
During the period from November 2018 to June 2019, a total of 12 sacropexies were performed at the Department of Minimally Invasive Gynecology of the Vyškov Hospital using the Seratex Slimsling method. Table 1 summarizes the data on surgical interventions. Table 2 summarizes the most important preoperative and perioperative data. Out of a total of 12 patients in the pilot study, 5 (41.7%) had a hysterectomy in the past, of which three were laparoscopically assisted and two were vaginal. In three cases, a laparoscopic assisted vaginal hysterectomy was performed at one time followed by a sling surgery of the vaginal stump with a Slimsling implant. In 4 (33.3%) patients, the uterus was left during the operation. In the same number of patients, the procedure was finished with concomitant anterior or posterior vaginal repair. 91.2% of the patients were multiparous, 95.7% of births were vaginal, with no use of VEX or forceps.
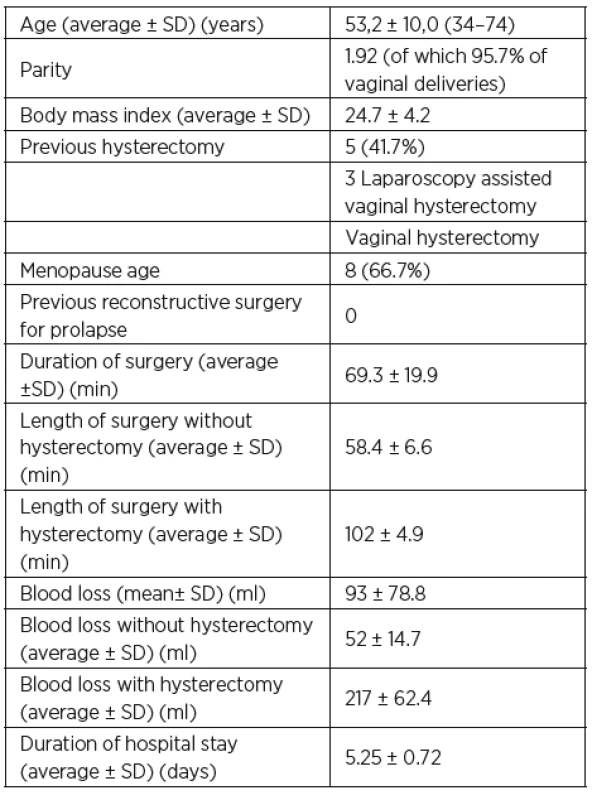
In the investigated group of patients, surgical times and blood loss differed significantly between patients with and without concomitant hysterectomy. Therefore, these data are different. The average time of an experienced surgeon in the case of the slimsling procedure without concomitant hysterectomy was about 58 minutes with an average blood loss of 52 ml. In three patients, concomitant hysterectomy prolonged surgery to an average of 102 minutes and blood loss averaged 217 ml.
Complications and folow up – peroperative complications
The surgery was complicated in one of the patients by the penetration of the vaginal mucosa and the necessity of subsequent extirpation and re-insertion of the implant. In one initial case, during the primary fixation phase on the sacrum, the implant was torn and replaced. There was no injury to large vessels or ureters and no conversion to laparotomy.
Complications and folow up – postoperative complications
Early postoperative period in one of the patients was complicated by uroinfection, treated by antibiotics. In one case, the implant failed and slipped from the sacrouterine ligaments area. Subsequently a vaginal stump prolapse three months after the primary operation occured. We explain this failure by incorrect surgical technique. The patient was subsequently re-operated six months after the primary operation using the same technique and is still without any problems. None of the patients suffered any protrusion of the implant or significant dyspareunias or discomfort during the follow-up period and, apart from the aforementioned patient, the method did not failed. None of the patients reported urinary incontinence during the postoperative period. Due to the recent termination of the study, we plan to continue to monitor the patients over a longer period of time.
DISCUSSION
Laparoscopic sacrocolpopexy is a safe and effective surgical treatment of genital prolapse [6, 12]. In our pilot study, we introduced a new method of this surgical technique using a Seratex Slimsling implant. In the examined group of 12 patients operated for pelvic organ prolapse, one patient (8.3%) registered a relapse in the postoperative period followed by successful reoperation using the same technique. Our data show a similar recurrence rate as reported in other studies [4, 12]. None of the performed operations was converted to laparotomy. Blood loss varied with a concomitant hysterectomy, averaging 217 ml versus an average of 52 ml blood loss in patients without concomitant hysterectomy. The mean blood loss in the whole group of patients was 93 ml. This blood loss is comparable to that of other laparoscopic sacrocolpopexy techniques [6]. We did not notice any infectious complication or protrusion in these patients partly because of careful implant placement in the area of the sacrouterine ligaments avoiding the surgical field after concomitant hysterectomy. Peroperative complications were related mainly to the new material and new surgical technique. A sling was torn in one case and vaginal mucosa was penetrated in another case. Both of these complications were repaired peroperatively by extraction and use of a new implant. During the follow up period there was no recurrence of prolapse, cystocele or rectocele. This fact may be influenced by the short postoperative follow-up.
Also, there was no postoperative protrusion of the implant. In the literature the vaginal protrusion after laparoscopic sacrocolpopexy is described in up to 11% [8, 11]. This demonstrates that the laparoscopic approach using Seratex Slimsling may be a safe method for surgical treatment of pelvic prolapse. With the use of the Serapro RTD the peritoneum dissection and its subsequent closure can be avoided. The tool is designed so that it can be used even in patients with higher BMI. The average time of surgery in an experienced surgeon´s hands is about 60 minutes in cases without concomitant hysterectomy. This surgery time is shorter than time reported in published studies [2, 6]. Short surgery time in our study may be related to the use of this new suspension tool requiring a minimum of tissue dissection. This pilot study is limited by a small number of operated patients. On the other hand, its strength can be seen in the mode of surgery which has been done in all patients by one experienced laparoscopic surgeon.
CONCLUSION
Based on our data, laparoscopic sacrocolpopexy using Seratex Slimsling implant seems to be an effective and fast method with a similar amount of relapses as other laparoscopic methods of pelvic organ prolapse. Thanks to the tools used, the surgery time can be shortened after learning the surgical technique. During the follow-up postoperative period, we did not register any mesh protrusion.
Poděkování
Tato publikace byla zpracována jako atestační práce za podpory a významného přínosu prof. MUDr. Radovana Pilky, Ph.D.
MUDr. Martin Vašíček
Gynekologické oddělení
Nemocnice
Purkyňova 235/36
682 01 Vyškov
e-mail: mvasicek89@gmail.com
Zdroje
1. Akl, MN., Long, JB., Giles, DL., et al. Robotic-assisted sacrocolpopexy: technique and learning curve. Surg Endosc, 2009, 23, p. 2390–2394.
2. Anger, JT., Mueller, ER., Tarnay, CH., et al. Robotic compared with laparoscopic sacrocolpopexy: A randomized controlled trial. Obstet Gynecol, 2014, 123(1), p. 5–12.
3. Arthure, HG., Savage, D. Uterine prolapse and prolapse of the vaginal vault treated by sacral hysteropexy. J Obstet Gynaecol Br Emp, 1957, 64(3), p. 355–360.
4. Bojahr, B., Tchartchian, G., Waldschmidt, M. Laparoscopic sacropexy: a retrospective analysis of perioperative complications and anatomical outcomes. JSLS, 2012, 16(3), p. 428–436.
5. Ganatra, AM., Rozet, F., Sanchez-Salas, R., et al. The current status of lapatoscopic sacrocolpopexy: a review. Eur Urol, 2009, 55(5), p. 1089–1103 Epub 2009 Feb 4.
6. Higgs, PJ., Chua, HL., Smith, AR. Long term review of laparoscopic sacropexy. BJOG, 2005, 112(8), p. 1134–1138.
7. Huguier, J., Scali, P. Posterior suspension of the genital axis on the lumbosacral disk in the treatment of uterine prolapse. La Presse Medicale, 1958, 66(35), p. 781–784.
8. Iglesia, CB., Fenner, DE., Brubaker, L. The use of mesh in gynecologic surgery. Int Urogynecol J Pelvic Floor Dysfunct, 1997, 8(2), p. 105–115.
9. Maher, C., Baessler, K., Glazener, CM., et al. Surgical management of pelvic organ prolapse in women, a short version of Cochrane review. Neurol Urodyn, 2008, 27(1), p. 3–12.
10. Manodoro, S., Werbrouck, E., Veldman, J., et al. Laparoscopic sacrocolpopexy. Facts Views Vis Obgyn, 2011, 3(3), p. 151–158.
11. Misrai, V., Rouprêt, M., Cour, F., et al. De novo urinary stress incontinence after laparoscopic sacral colpopexy. BJU Int, 2008, 101(5), p. 594–597.
12. North, C., Ali-Ross, N., Smith, A., Reid, FM. A prospective study of laparoscopic sacropexy for the management of pelvic organ prolapse. BJOG, 2009, 116(9), p. 1251–1257.
13. Pilka, R., Gagyor, D., Študentová, M., Neubert, D., Dzvinčuk, P. Laparoscopic and robotic sacropexy: retrospective review of learning curve experiences and follow-up. Čes Gynek, 2017, 76, p. 261–265.
Štítky
Dětská gynekologie Gynekologie a porodnictví Reprodukční medicínaČlánek vyšel v časopise
Česká gynekologie

2019 Číslo 6
Nejčtenější v tomto čísle
- Histopathological and clinical features of molar pregnancy
- Prenatally diagnosed patent urachus with umbilical cord cyst and early surgical intervention
- The incidence of gestational diabetes mellitus before and after the introduction of HAPO diagnostic criteria
- The effect of physiotherapy intervention on the load of the foot and low back pain in pregnancy