Effect of umbilical cord drainage after spontaneous delivery in the third stage of labor
Vplyv drenáže pupočníka po spontánnom pôrode na tretiu dobu pôrodnú
Drenáž pupočníka zahŕňa uvoľnenie Peánových klieští z pupočníka po oddelení novorodenca z maternálneho konca pupočníka. Následne dochádza k vyprázdňovaniu krvi z placenty. Tento postup je súčasťou aktívneho vedenia III. doby pôrodnej (TSL – third stage of labor). Cieľ: Táto štúdia je určená na poskytnutie poznatkov o dĺžke trvania tretej doby pôrodnej a riziku retencie placenty pri použití drenáže pupočníka, a pri postupe bez drenáže pupočníka. Materiál a metodika: Prospektívnej randomizovanej štúdie manažmentu TSL sa zúčastnilo 600 pacientiek. Pacientky boli rovnomerne rozdelené do dvoch skupín s drenážou pupočníka (300) a bez drenáže pupočníka (300). TSL bola aktívne vedená odporúčaniami FIGO (the International Federation of Gynecology and Obstetrics). Sledovali sme trvanie TSL a retenciu placenty po 30 min. Výsledky: Priemerné trvanie TSL bolo 6,8 ± 0,4 min v skupine s drenážou a 11,6 ± 0,8 min v kontrolnej skupine. Dospeli sme k záveru, že drenáž pupočníka významne skracuje trvanie TSL (p = 0,026), ako aj znižuje riziko retencie placenty. V skupine, s použitou drenážou pupočníka sa retencia placenty 30 min po pôrode plodu vyskytla v čtyroch prípadoch, kým v druhom súbore sa vyskytla v 14 prípadoch (RR 3,62; 95% CI 1.18–11.14). Záver: Predpokladáme, že pri drenáži pupočníka dochádza ku kolabovaniu tenkostenných uteroplacentárnych ciev skôr, čo spôsobuje krvácanie z týchto ciev medzi placentu a stenu maternice, a týmto mechanizmom dochádza k včasnejšiemu odlúčeniu placenty. Samozrejme, že drenáž pupočníka je len jedným z krokov algoritmu aktívneho vedenia tretej doby pôrodnej podľa FIGO.
Klíčová slova:
III. doba pôrodná – drenáž placenty – manuálne vybavenie placenty – popôrodné krvácanie – retinovaná placenta
Authors:
Erik Dosedla 1
; Petra Gašparová 1
; Zuzana Ballová 1
; Martina Sitáš 1
; P. Calda 2
Authors place of work:
Department of Gynaecology and Obstetrics, Faculty of Medicine, Pavol Jozef Safarik University in Kosice and Hospital Agel Košice-Šaca Inc., Košice-Šaca, Slovak Republic
1; Department of Gynaecology, Obstetrics and Neonatology, First Faculty of Medicine Charles University and General Teaching Hospital, Prague, Czech Republic
2
Published in the journal:
Ceska Gynekol 2023; 88(4): 260-263
Category:
Původní práce
doi:
https://doi.org/10.48095/cccg2023260
Summary
Umbilical cord drainage involves releasing the cord clam from the umbilical cord after separation of the newborn from the maternal end of the umbilical cord. Consequently, there is emptying of blood from the placenta. This procedure is part of the active management of the third stage of labor (TSL). Objective: This study is intended to provide knowledge about the duration of TSL and the risk of retention of the placenta using umbilical cord drainage and the no-drainage procedure. Materials and methods: A prospective randomized study of the management of the third stage of labor in 600 patients. The patients were equally divided into two groups with umbilical cord drainage (300) and without umbilical cord drainage (300). TSL was actively managed by FIGO (the International Federation of Gynecology and Obstetrics) recommendations. We monitored the duration of TSL and retention of the placenta after a 30 min period. Results: The mean duration of TSLwas 6.8 ± 0.4 min in the drainage group and 11.6 ± 0.8 min in the control group. We conclude that umbilical cord drainage significantly shortens the duration of TSL (P = 0.026) as well as reduces the risk of placental retention. In a group where we use the drainage of the umbilical cord, placental retention 30 min after delivery of the fetus occurred in four cases while the second set occurred in 14 cases (RR 3.62; 95% CI 1.18–11.14). Conclusion: We assume that during umbilical cord drainage, the collapse of thin-walled uteroplacental vessels occurs earlier causing bleeding from these vessels between the placenta and the uterine wall, and therefore, earlier separation of the placenta occurs. Of course, the drainage of the umbilical cord is only one step in the algorithm of active management at the third stage of labor according to FIGO.
Keywords:
Postpartum hemorrhage – retained placenta – third stage of labor – placental cord drainage – manual removal of placenta
Introduction
The third stage of labor (TSL) is defined as the period from the delivery of the fetus to the expulsion of the placenta [1], which in average lasts between 6 and 30 min. Currently, there is still a lack of full understanding of the physiology of TSL. Expulsion of the placenta with the formation of capillary hemorrhage and retroplacental hematoma after the birth of the fetus is followed by shrinking of the placental surface with uterine contractions, and finally ends with the delivery of the placenta from the uterus. It is associated with some form of hemorrhage which is reduced by uterine contractions and activation of the coagulation system (myotamponade and thrombotamponade) [2]. Proper management of TSL makes it possible to avoid or at least reduce postpartum hemorrhage (PPH) [3].
PPH is defined as blood loss of 500 mL or more within 24 h after delivery and most frequently occurs during the third or fourth stage of labor (2 h postpartum) [4,5]. The prevalence of PPH (blood loss ≥ 500 mL) is approximately 6.0–10.0%, and the prevalence of severe PPH (blood loss ≥ 1,000 mL) is approximately 1.8–3.0% in any type of delivery, but varies by region worldwide [5]. PPH is the most common cause of maternal mortality, especially in under-developed countries and accounts for about 25% of maternal deaths. In addition to mortality, PPH may result in inadequate lactation, iron deficiency anemia, coagulopathy and exposes patients to needing a blood transfusion. Therefore, adequate management of TSL is a crucial tool in the prevention of complications where the amount is increasing exponentially, especially if the duration of TSL is extended. There are many obstetric risk factors for a prolonged third stage, including advanced maternal age, nulliparity, extreme obesity, intrapartum fever, and multiple gestation [6]. The most dangerous complications are postpartum bleeding due to uterine atony, retention of a cotyledon or the entire placenta. Retained placenta was defined as a placenta that was not delivered within 30 min of delivery and is the most common cause of postpartum hemorrhage [7]. Retained placenta is a complication encountered in approximately 0.5–3% of deliveries [7–9]. Subsequent manual removal of the placenta is often complicated by bleeding, infection or trauma to the cervix or vagina as well as those risks associated with the type of anesthetic [9].
The management of TSL in Slovakia follows recommended procedures (FIGO – the International Federation of Gynecology and Obstetrics – guidelines) guidelines) and involves active management. Administration of prophylactic doses of uterotonic drugs (oxytocin) after delivery of the anterior shoulder of the baby or after the expulsion of the placenta, early umbilical cord clamping and its cutting and then delivery of the placenta by controlled umbilical cord traction combined with maternal effort. On the other hand, TSL could be managed by the expectant management, in which no uterotonics are administered, the umbilical cord is clamped only after the umbilical cord pulsation stops and the placenta is delivered spontaneously with the aid of gravity, sometimes by maternal effort or nipple stimulation [10]. This expectant management is not the standard procedure in Slovakia. There is evidence that active management of TSL reduces the incidence of postpartum hemorrhage by approximately 65% compared with expectant management [11].
Umbilical cord drainage (UCD) as a part of active management of TSL is effective in reducing duration, blood loss, and the incidence of PPH [12,13]. It is a simple, safe, and non-invasive approach. UCD is defined as the unclamping of the maternal side of the umbilical cord, thereby permitting the blood from the placenta to drain freely into a vessel immediately after the clamping and cutting of the umbilical cord [14]. It involves draining the blood from the placenta into a suitable collection container (kidney tray).
Materials and methods
UCD is another option for FIGO’s series of recommended procedures for active management of TSL. Our aim was to gain knowledge about the duration of TSL and the risk of placental retention using a procedure with UCD and without UCD. We submitted a group of 600 low- -risk pregnant women to the prospective study. We used simple randomization by assigning subjects into two groups for every assignment. TSL was performed with active management via FIGO recommendations. In a group of 300 patients with primary vaginal delivery, without selection biases, we used the UCD procedure. In the second group of 300 patients, TSL was managed without UCD. In the above groups, we monitored the length of TSL and the frequency of placental retention after 30 min from the beginning of TSL.
We used the statistical program Wizard 2 version 2.0.12 to analyze the results. We used the following analytical methods for the statistical analysis: descriptive analysis, Mann-Whitney U-test and relative risk (RR). We considered a value of P < 0.05 to be statistically significant.
Results
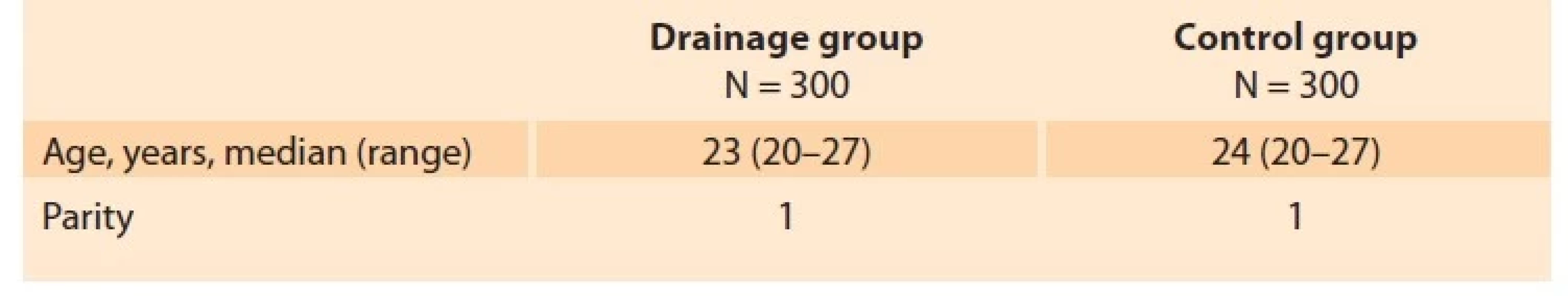
The total number of 600 patients in active labor were enrolled in the trial. They were equally distributed into two groups. Statistical analysis of demographic and clinical data revealed the following results: the median age of the patients in the drainage group and no drainge group was 23 and 24 years, respectively (range 20–27 years).
The median age in the drainage group was higher compared to the drainage group. All of them were primiparas (Tab. 1). The mean duration of TSL in the drainage group was 6.8 ± 0.3 min and in the control group it was 11.6 ± 0.8 min. The median duration of TSL was statistically lower in the drainage group (P = 0.026). In the group using UCD, we observed placental retention in four (1.3%) cases but 14 (4.7%) cases in the control group (Tab. 2).
Tab. 1. Demografická charakteristika sledovanej populácie.
Tab. 2. Dĺžka tretej doby pôrodnej a retencia placenty v jednotlivých skupinách.
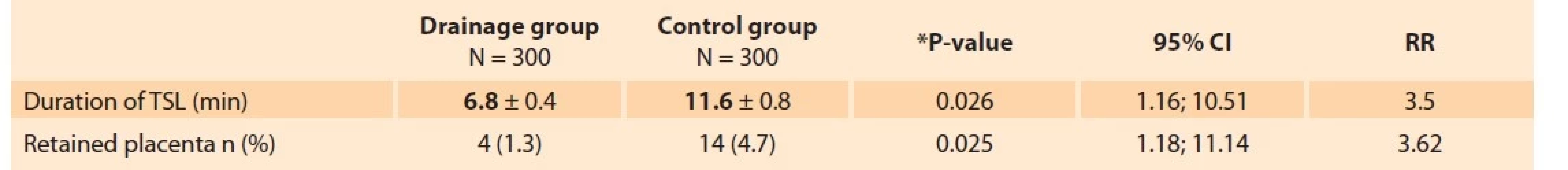
RR – relative risk assessment, TSL – third stage of labor
Discussion
Active management of TSL remarkably reduced the duration of TSL [3,12]. It showed a significant decrease in primary blood loss greater than 500 mL, and mean maternal blood loss at birth, maternal blood transfusion and therapeutic uterotonics during the third stage or within the first 24 h, or both [11]. Active management may reduce the incidence of maternal anemia (Hb less than 90 g/L) following birth [15]. However, active treatment has increased the incidence of postpartum diastolic blood pressure above 90 mmHg, nausea, and vomiting (probably due to the use of ergometrine-based uterotonics), postpartum pain, the need for postpartum analgesia and an increase in the number of women who must return to hospital due to bleeding [2,10].
Several studies have been performed to assess UCD as part of active TSL management. Their main aim was to assess its effect on the duration of TSL, the volume of blood loss, and the need for manual placental lysis. In 1999, Razmkhah et al first reported that the duration of TSL could be shortened via UCD [16]. Asicioglu announced that UCD during TSL is associated with reduced blood loss during the third and fourth stages of labor (70 mL) [12]. Roy described the incidence of postpartum hemorrhage in 1% of women with UCD and in 9% of women without drainage [13]. However, there were also opponents of this method, such as Vasconcelos et al, who disclosed that UCD had no effect in reducing duration or blood loss during the third stage of labor [17].
In our study, we observed the duration of TSL. In the study group with UCD, the median duration of TSL was 6.8 ± 0.4 min while in the control group without drainage it lasted 11.6 ± 0.8 min; the difference was statistically significant. Remarkable shortening of TSL using UCD was also demonstrated in other studies. In a cohort of 485 female patients randomly assigned to two groups with similar demographic and clinical baseline characteristics, another group of authors evaluated UCD as effective in reducing the duration of TSL. It was shortened by 4.2 min (3.5 ± 1.9 vs. 7.7 ± 3.4, respectively) [12]. In a study by Roy et al in a cohort of 200 patients, the median duration of TSL was 210.5 s in the study group with drainage and 302.5 s in the control group [13].
We noticed placental retention 30 min after delivery of the fetus in four cases (1.3%) in the drainage group, while in the control group without drainage placental retention occurred in 14 cases (4.7%). In a study by Asicioglu et al, 0.8% of placentas in the drainage group and 4.5% in the second group without drainage remained undelivered beyond 15 min. In their study, neither placental retention nor the need for manual lysis occurred [12].
In a recent randomized trial, a remarkable decrease in placental expulsion time (7.09 ± 1.01 vs. 10.43 ± 3.20 min, P < 0.001) was also demonstrated as well as reduction of manual removal of the placenta, retained placenta and postpartum hemorrhage in the study group with UCD [18].
We assume that after UCD, there is earlier bleeding from thin-walled uteroplacental vessels between the placenta and the uterine wall and it can accelerate placental separation. Continuous uterine contraction and retraction in TSL lead to reduction of uterine size, the placenta becomes inelastic, and it gets separated from the uterus. UCD makes the placenta smaller and compact, which enhances early separation and delivery with less blood-loss [1]. The discharge of blood from the placental bed with the use of the cord drainage method may reflect the stimulation of myometrial contractions and a decrease in the area of placental adherence. This mechanism may also help induce placental expulsion. Stimulation of myometrial contractions also explains the reduced need for uterotonic agents after UCD [12].
In our study, we noted no adverse events, such as hypotension or vasovagal syncope, associated with the use of the umbilical cord drainage method. We also did not find any UCD-related side events reported in other studies.
Conclusion
Routine active management obviously reduces blood loss, PPH and other serious complications resulting from TSL despite being associated with a higher risk of side effects such as nausea and vomiting, and elevation of blood pressure after ergotaminutese administration. Active TSL management is routine in vaginal deliveries. It does not affect the fetus and the newborn. UCD as part of active management after fetal delivery shortens the duration of TSL and reduces the risk of retained placenta. With present signs of placental separation, the delivery of the placenta is completed by controlled umbilical cord traction. Controlled traction is safe and is the third component after administration of uterotonics and interruption of clamping the umbilical cord. Excessive zeal of the obstetrician with careless traction or fundamental pressure is not only painful but can lead to interruption of the separation of the uteroplacental vessels, separation of the placenta, ending with the inversion of the uterus. Umbilical cord drainage is a safe method that shortens the duration of TSL and reduces the risk of obstetric complications.
ORCID authors
E. Dosedla 0000-0001-8319-9008
P. Gašparová 0000-0002-6354-6911
Z. Ballová 0000-0002-0605-948X
M. Sitáš 0000-0002-7273-1051
P. Calda 0000-0002-2903-5026
Submitted/Doručené: 2. 1. 2023
Accepted/Prijaté: 11. 5. 2023
Assoc. Prof. Erik Dosedla, MD, PhD, MBA
Department of Gynaecology and Obstetrics
Faculty of Medicine
Pavol Jozef Safarik University
Hospital Agel Košice-Šaca Inc.
Lúčna 57
040 15 Košice-Šaca
Slovak Republic
Zdroje
1. Afzal MB, Bushra N, Waheed K et al. Role of placental blood drainage as a part of active management of third stage of labour after spontaneous vaginal delivery. J Pak Med Assoc 2019; 69 (12): 1790–1793. doi: 10.5455/JPMA.302642458.
2. Güngördük K, Olgaç Y, Gülseren V et al. Active management of the third stage of labor: a brief overview of key issues. Turk J Obstet Gynecol 2018; 15 (3): 188–192. doi: 10.4274/tjod.39 049.
3. Yildirim D, Ozyurek SE, Ekiz A et al. Comparison of active vs. expectant management of the third stage of labor in women with low risk of postpartum hemorrhage: a randomized controlled trial. Ginekol Pol 2016; 87 (5): 399–404. doi: 10.5603/GP.2016.0015.
4. Raams TM, Browne JL, Festen-Schrier VJ et al. Task shifting in active management of the third stage of labor: a systematic review. BMC Pregnancy Childbirth 2018; 18 (1): 47. doi: 10.1186/ s12884-018-1677-5.
5. Masuzawa Y, Kataoka Y, Fujii K et al. Prophylactic management of postpartum haemorrhage in the third stage of labour: an overview of systematic reviews. Syst Rev 2018; 7 (1): 156. doi: 10.1186/s13643-018-0817-3.
6. Whittington JR, Pagan M, Daugherty K et al. Duration of the third stage of labor and estimated blood loss in twin vaginal deliveries. AJP Rep 2020; 10 (3): e330–e334. doi: 10.1055/ s-0040-1715170.
7. Grillo-Ardila CF, Amaya-Guio J, Ruíz-Parra AI et al. Systematic review of prostaglandin analogues for retained placenta. Int J Gynaecol Obstet 2018; 143 (1): 19–23. doi: 10.1002/ijgo.12572.
8. Anteby M, Many A, Ashwal E et al. Risk factors and complications of manual placental removal after vaginal delivery – how common are additional invasive procedures? J Matern Fetal Neonatal Med 2019; 32 (3): 384–388. doi: 10.1080/14767058.2017.1379071.
9. Djakovic I, Djakovic Z, Bilić N et al. Third stage of labor and acupuncture. Med Acupunct 2015; 27 (1): 10–13. doi: 10.1089/acu.2014.1079.
10. Begley CM, Gyte GM, Devane D et al. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev 2015; 3: CD007412. doi: 10.1002/14651858.CD007412.pub.4.
11. Du Y, Ye M, Zheng F. Active management of the third stage of labor with and without controlled cord traction: a systematic review and meta-analysis of randomized controlled trials. Acta Obstet Gynecol Scand 2014; 93 (7): 626–633. doi: 10.1111/aogs.12424.
12. Asicioglu O, Unal C, Asicioglu BB et al. Influence of placental cord drainage in management of the third stage of labor: a multicenter randomized controlled study. Am J Perinatol 2015; 32 (4): 343–350. doi: 10.1055/s-0034-1384639.
13. Roy P, Sujatha MS, Bhandiwad A et al. Placental blood drainage as a part of active management of third stage of labour after spontaneous vaginal delivery. J Obstet Gynaecol India 2016; 66 (Suppl 1): 242–245. doi: 10.1007/s132 24-016-0857-3.
14. Wu HL, Chen XW, Wang P et al. Effects of placental cord drainage in the third stage of labour: a meta-analysis. Sci Rep 2017; 7 (1): 7067. doi: 10.1038/s41598-017-07722-7.
15. Begley CM, Gyte GM, Devane D et al. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev 2019; 2 (2): CD007412. doi: 10.1002/ 14651858.CD007412.pub5.
16. Razmkhan N, Kordi M, Yousophi Z. The effects of cord drainage on the length of third stage of labour. J Nurs Midwifery 1999; 1: 10–14.
17. Vasconcelos FB, Katz L, Coutinho I et al. Placental cord drainage in the third stage of labor: randomized clinical trial. PLoS One 2018; 13 (5): e0195650. doi: 10.1371/journal.pone.0195650.
18. Karimi N, Molaee G, Esfahani NT et al. Placental cord drainage and its outcomes at third stage of labor: a randomized controlled trial. BMC Pregnancy Childbirth 2022; 22 (1): 570. doi: 10.1186/s12884-022-04877-8.
Štítky
Dětská gynekologie Gynekologie a porodnictví Reprodukční medicínaČlánek vyšel v časopise
Česká gynekologie
2023 Číslo 4
Nejčtenější v tomto čísle
- The efficacy of human papillomavirus vaccination in the prevention of recurrence of severe cervical lesions
- Therapeutical strategies for recurrent endometrial cancer
- Direct abdominal muscle diastasis and stress urinary incontinence in postpartum women
- Effect of umbilical cord drainage after spontaneous delivery in the third stage of labor
