Primární maligní melanom pochvy, kazuistika a review z literatury
Primary malignant melanoma of the vagina, case report and review of the literature
Objective:
Presentation of primary malignant melanoma of the vagina. Summary of clinical findings and management.
Design:
Case report.
Setting:
Nemocnice Pardubického kraje a.s., Porodnicko-gynekologická klinika, Pardubice.
Observation:
We report a case of primary malignat melanoma in a 44 year old woman, with symptoms of abnormal vaginal bleeding and painful intercourse.
Conclusion:
Primary malignant melanoma of the vagina is rare disease. Goal of therapy is complete removal of primary tumor.
Keywords:
malignant melanoma, vagina
Authors:
J. Göbel 1; M. Košťál 1; G. Hensel 1; J. Hátlová 2
Authors‘ workplace:
Porodnicko-gynekologická klinika Nemocnice Pardubického kraje, přednosta doc. MUDr. M. Košťál, CSc.
1; Patologické oddělení Nemocnice Pardubického kraje, primářka MUDr. M. Hácová
2
Published in:
Ceska Gynekol 2018; 83(3): 201-199
Overview
Cíl studie:
Prezentace kazuistiky primárního maligního melanomu pochvy. Shrnutí klinických nálezů a management.
Typ studie:
Kazuistika.
Název a sídlo pracoviště:
Nemocnice Pardubického kraje a.s., Porodnicko-gynekologická klinika, Pardubice.
Vlastní pozorování:
V kazuistice popisujeme případ primárního maligního melanomu pochvy u 44leté ženy, který se projevil abnormálním vagináním krvácením a bolestí při styku.
Závěr:
Primární maligní melanom pochvy je vzácné onemocnění. Cílem léčby je kompletní odstranění primárního ložiska.
Klíčová slova:
maligní melanom, pochva
INTRODUCTION
Malignant melanoma is considered to arise from melanocytic cells in the skin and mucosal membranes. Malignant melanomas predominantly develop in areas that are exposed to sunlight. Primary malignant melanoma of the vagina (PMMV) is extremely rare and aggressive tumor with less than 300 cases reported worldwide [2]. Incidence is only 0.46 per one million women per year [6]. It accounts less than 1% of all melanomas in women, and less than 3% of all vaginal malignancies [15]. PMMV is a lesion of poor prognosis, even more serious than cutaneous localizations, such as vulvar melanoma. Survival five year rate is around 18% [10]. PMMV usually occurs in women aged in their 60s or 70s, with the majority of patients being postmenopausal [10]. Patient commonly complains of vaginal bleeding, vaginal discharge or a palpable mass. In our case we present PMMV in premenopausal woman.
CASE REPORT
A 44 year old female was admitted to the Department of Obstetrics and Gynecology, county hospital Pardubice with complaint of irregular vaginal bleeding and painful intercourse for the last month. Clinical examination identified solid ulcerated tumor 2 cm in diameter behind vaginal introitus at number 4. Color of tumor was brown-grey. Tumor was resected in local anesthesia. Pathological and imunohistochemical analyses confirmed nodular malignant melanoma, Breslow 1.9 mm. Oncogynecological group recommended further therapy.
Three weeks after local excision two new superficial hyperpigmeted lesions arose above place of excision (figure 1) and the patient underwent wide local excision of the vagina – to achieve further radicallity urethrectomy will be necessary. Patient also underwent the sentinel lymph node mapping with technetium and blue dye injection. Sentinel node was found around left external iliac artery and left inquinofemoral lymphadenectomy was also performed.
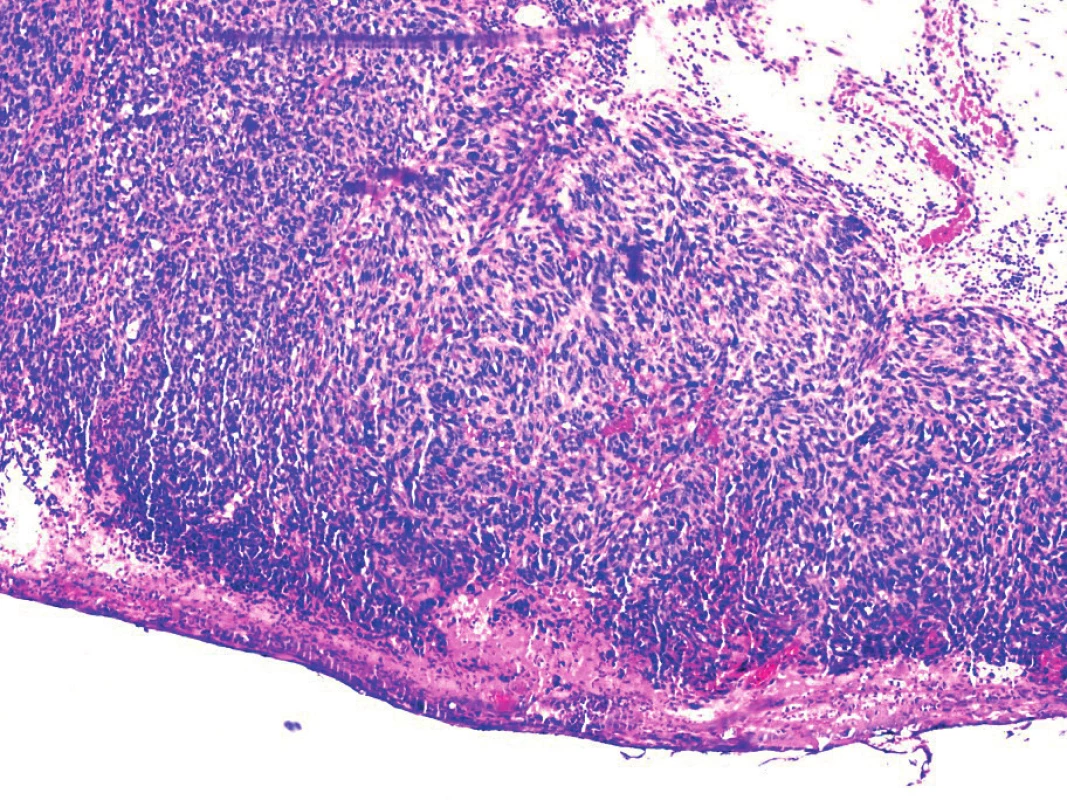
Pathological analyses revealed in section of vagina (figure 2) residual malignant melanoma with superficial dissemination, but all surgical margins were clear of tumor. Biopsy of the sentinel node was negative, as well as 10 lymphatic nodes from left groin.

Oncogynecological group recommended adjuvant therapy with interferon α-2b. The patient underwent complex dermatological examination with excision of seven pigment marks from trunk, which were all negative. After fifth dose of interferon the patient refused further therapy because of severe adverse effects and was lost to follow up three months after surgery.
DISCUSSION
Primary malignant melanoma of the vagina is rare gynecological malignancy that is associated with high risk of recurrence, distant metastases and short survival rate. The tumor is most frequently located in the distal third of anterior vaginal wall [3]. Prognostic factors are tumor size, depth of invasion, lymph node status, extent of surgery and adjuvant therapy. Buchannan et al. showed in meta-analysis, that there is a significant difference in average survival time between patients with tumor diameters of < 3 cm and ≥ 3 cm [2]. Vaginal malignant melanomas are commonly pigmented but occasionally may be devoid of pigment or may contain both pigmented and non-pigmented lesions [8]. Staging of PMMV is usually confused with that of vaginal carcinoma and cutaneous melanoma, which do not reflect the poorer prognosis of PMMV. Appropriate and effective treatment protocols for PMMV have not been established. Surgery, radiotherapy and immunotherapy are recommended as individual and combined therapies. Surgery remains the optimal treatment and is considered to be the only potentially curative treatment for PMMV.
Surgical management for primary disease ranges from conservative local excision to a more radical approach including vaginectomy and pelvic exenteration. The relationship between survival and extent of surgery has not been proven. Some oncosurgeons maintain radical surgery as preferred approach to reduce local recurrence risk and improve survival [4, 14]. Recent reports have argued that wide local excision can achieve equivalent survival rates [1, 8, 12]. Treatment should be individualized, if local excision is impossible, radical surgery should be performed to completely remove the tumor.
The role of lymphadenectomy in vaginal melanoma remains under debate. Recent studies have shown that lymphadenectomy is not essential for the low rate of regional lymph node metastasis and significant morbidity [2, 7, 12]. Sentinel lymph node biopsy to confirm node status is essential in improving the accuracy of staging. Due to its low morbidity, it has recently gained popularity in both cutaneous and vaginal melanomas [1, 11].
Radiotherapy has limited benefit in improving the overall survival but may be of value as the adjuvant treatment following surgery or primarily for tumors that cannot be removed surgically. The effect of chemotherapy as primary or adjuvant therapy on patient survival has not been determined. Traditional cytotoxic agents, including platinum compounds either alone or in combination, have been evaluated as being of limited or no benefit in the treatment of melanoma [13].
BRAF mutations in vulvovaginal melanomas are more common than in cutaneous melanomas, that render this disease as distinct subtype of melanoma [5]. Currently only one immunoagent for surgically resected melanomas is interferon α-2b but it has not been formally studied in mucosal melanoma, although it is frequently offered to these patients. Clinical trials have focused on molecular targeting therapy. Agents ipilimumab and vemurafenib are approved by the US Food and Drug Administration for unresectable or metastatic cutaneous melanoma [15].
CONCLUSION
Although primary vaginal melanoma is rare malignant disease, attention should be given to suspicious pigmented lesions in routine gynecological examinations. Depth of invasion and lymph node status are important determinants of survival for PMMV. No consensuses have been achieved regarding optimal management, but complete removal of primary tumor is the major premise. Adjuvant therapy may be goal for further investigation on large sample size.
MUDr. Jindřich Göbel
Porodnicko-gynekologická klinika
Nemocnice Pardubického kraje a.s.
Kyjevská 44
530 12 Pardubice
e-mail: j.gobel@volny.cz
Sources
1. Arenbergerová, M., Fialová, A., Pojezná, E. Melanom vulvy. Čes Gynek, 2013, 78, 4, s. 351–355.
2. Buchanan, D., Schlaerth, J., Kurosaki, T. Primary vaginal melanoma: thirteen-year disease-free survival after wide local excision and review of recent literature. Am J Obstet Gynecol, 1998, 178(6), p. 11.
3. Chen, L., Xiong, Y., Wang, H., et al. Malignant melanoma of the vagina: a case report and review of the literature. Oncol Lett, 2014, 8(4), p. 1585–1588. Epub 2014 Jul 17.
4. Geisler, JP., Look, KY., Moore, DA., Sutton, GP. Pelvic exenteration for malignant melanomas of the vagina or urethra with over 3 mm of invasion. Gynecol Oncol, 1995, 59(3), p. 338–341.
5. Hu, DN., Yu, GP., McCormick, SA. Population-based incidence of vulvar and vaginal melanoma in various races and ethnic groups with comparisons to other site-specific melanomas. Melanoma Res, 2010, 20(2), p. 153–158.
6. Mario, M., Leitao, J. Management of vulvar and vaginal melanomas: current and future strategies. ASCO Educational book 2014.
7. Miner, TJ., Delgado, R., Zeisler, J., et al. Primary vaginal melanoma: a critical analysis of therapy. Ann Surg Oncol, 2004, 11(1), p. 34–39.
8. Oguri, H., Izumiya, C., Maeda, N., et al. A primary amelanotic melanoma of the vagina, diagnosed by immunohistochemical staining with HMB-45, which recurred as a pigmented melanoma. J Clin Pathol, 2004, 57(9), p. 986–988.
9. Ragnarsson-Olding, B., Johansson, H., Rutqvist, LE., et al. Malignant melanoma of the vulva and vagina. Trends in incidence, age distribution, and long-term survival among 245 consecutive cases in Sweden 1960–1984. Cancer, 1993, 71(5), p. 1893–1897.
10. Rob, L., Robová, H., Pluta, M., et al. Detekce sentinelových uzlin u karcinomu vulvy – metody a technika. Čes Gynek, 2006, 71(4), s. 298–301.
11. Sugiyama, VE., Chan, JK., Kapp, DS. Management of melanomas of the female genital tract. Curr Opin Oncol, 2008, 20(5), p. 565–569.
12. Tjalma, WA., Monaghan, JM., de Barros Lopes, A., et al. Primary vaginal melanoma and long-term survivors. Eur J Gynaecol Oncol, 2001, 22(1), p. 20–22.
13. Van Nostrand, KM., Lucci, JA., Schell, M., et al. Primary vaginal melanoma: improved survival with radical pelvic surgery. Gynecol Oncol, 1994, 55(2), p. 234–237.
14. Xia, L., Han, D., Yang, W., et al. Primary malignant melanoma of the vagina: a retrospective clinicopathologic study of 44 cases. Inter J Gynecol Cancer, 2014, 24(1), p. 149–155.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicineArticle was published in
Czech Gynaecology

2018 Issue 3
Most read in this issue
- Prolaktin a poruchy reprodukce
- Ovlivňuje použití transferového média EmbryoGlue úspěšnost embryotransferu?
- Vakcinace proti HPV a výhled nových možností
- Plánovaný domácí porod – Česká republika 2018
